Low-Glycemic Eating Made Easy—Combining Foods for Stable Glucose

Key Takeaways
The glycemic index (GI) ranks foods by how quickly they raise your glucose; essentially showing which foods give you steady energy and which ones lead to crashes.
Highlights:
- You can steady your energy after meals by pairing carbs with protein, fiber, or healthy fats: small tweaks that keep your glucose (and mood) more balanced.
- See the charts below for examples of high, moderate, and low-glycemic foods to guide your choices.
- The Nutrisense program, which uses a biosensor to track your personal glucose responses, is currently available only in the United States.
The glycemic index (GI) ranks foods by how quickly they raise your glucose; essentially showing which foods give you steady energy and which ones lead to crashes.
Highlights:
- You can steady your energy after meals by pairing carbs with protein, fiber, or healthy fats: small tweaks that keep your glucose (and mood) more balanced.
- See the charts below for examples of high, moderate, and low-glycemic foods to guide your choices.
- The Nutrisense program, which uses a biosensor to track your personal glucose responses, is currently available only in the United States.
All food gives you energy, of course. However, not all energy lasts. Some foods fuel you evenly, while others cause a quick spike and crash. This energy enters our blood as glucose, a simple sugar that our organs use to power their metabolism and support ours. When we look at different foods, one way to compare how our bodies will handle their energy is to calculate their glycemic index (GI).
What is a glycemic index chart?
Foods with lower GI values help your body stay balanced longer: no more post-meal fatigue or snack cravings an hour later. When your glucose spikes and drops quickly, you feel it: the energy dip, the irritability, the sudden hunger. Learning to smooth those curves with a holistic health plan helps you feel more stable day to day.
If you replace foods high in starch and have relatively high GI values with foods digested more slowly or have less starch to digest, the result will be a more even level of glucose over the day.
Which factors change GI response
Typically, foods will change over time, which is why they have sell-by and eat-by dates. Fruits and vegetables usually contain a lot of starch, but this starch breaks down into sugars over time. In fact, as some of this sugar ferments, it forms alcohol. There are some hypotheses that we like alcohol because it’s associated with a more readily available source of sugar in nature.
Even simple choices (like how ripe your fruit is) can change your body’s response. An apple fresh off the tree won’t hit your system quite the same as one that’s been sitting on the counter all week. If you’re looking at oven fries, the GI will most likely be as advertised. But fruits and vegetables will do some digestion for us the longer they are left to ripen, and you can find a chart of different options and their GIs here.
Why do GI responses differ by person
Although a food’s GI value provides valuable information for planning your diet, we need to know more to understand the physiologic effects of nutrition on your glucose levels. The standard GI chart is based on population averages, but your body may react differently. What spikes one person’s glucose may barely nudge another’s.
For any individual, though, their unique responses to a given food are what matter for their health, not how the food generally affects other people on average. The GI is, of course, sound and valuable as a guide, but it would be even better to know how a food will affect a specific person.
What else matters beyond GI
There is also a wide range of nutritional information that can make food good or bad for us, or more specifically, for a person. Generally, foods that provoke smaller glucose responses are also better for weight control, but not always.
For instance, vegetable oils barely affect your glucose but can still add up calorie-wise. That’s why glucose is one clue, not the whole picture. Trade-offs like this are abundant in nutrition, and no one figure, however useful on its own, will be the definitive factor for every person.

How is the glycemic index measured
Researchers calculate GI by measuring glucose for two hours after eating a food—but those lab averages don’t always predict your personal response. The total rise in glucose levels over those two hours is then compared with the effect of pure glucose on that same person’s blood glucose levels over the same two hours. The resulting ratio is the GI for that food, 100 for pure glucose, as the two levels would be the same.
For something like a low-starch vegetable, it could be much lower. The sample size is at least ten people, and the amount of food tested is typically fifty grams. Remember, the lower the GI of a specific food, the slower or lower the rise in glucose levels, so foods with a high GI will have a harsher effect on glucose levels.
What counts as low, moderate, and high GI
A food is considered to have a low glycemic index if its GI is below 55, which means it will release about half as much glucose into the blood over the first 2 hours. Likewise, a food is considered to have a high glycemic index if the GI is over 70, while values between 55 and 70 are considered moderate. For example, if you follow a keto diet, using the GI can be a valuable starting point for choosing foods that work well for you.
Smart food combination strategies
Adjusting how and when you eat carbs is one of the simplest ways to see big changes in how you feel after meals. Try one change at a time and review your post-meal patterns.
- Protein and veggies first, carbs last. Start with leafy greens dressed with olive oil, then add a protein like eggs, chicken, tofu, or fish, and finally eat the starch or fruit.
- Pair carbs with fiber. Add lentils or beans to rice, or berries to plain yogurt.
- Add healthy fats in moderation. Try avocado with whole-grain toast, or sprinkle almonds over steel-cut oats.
- Add acidity. Use a vinaigrette with vinegar or a squeeze of lemon on salads, rice, or potatoes.
- Choose whole food carbs. Pick intact grains like quinoa or steel-cut oats over refined options, and whole fruit like berries instead of juice.
Try a mini experiment in the Nutrisense App. Your biosensor measures glucose in interstitial fluid. Try two versions of the same meal on different days and compare your 2-hour curve in the app. This helps you see how macronutrient sequencing and pairing work for you.
As we said above, the GI of a specific food is altered by many factors, including how it’s prepared, processed, and eaten in combination with other foods. Since the GI is calculated from a 50-gram sample, the amount of food eaten at a single meal is also relevant.
Find the right Nutrisense programto turn insight into progress.
You’re already eating well. Now see which foods actually work for you
You’re already eating well. Now see which foods actually work for you
Glycemic index vs glycemic load: how do they differ
To address this last problem (that most people will not eat exactly 50 grams of a specific food at once), we can use the glycemic load (GL) to paint a more realistic picture of a food’s effect on glucose levels.
To get this value, we start with the GI, which is accurate while remaining agnostic to the amount of food eaten. We then multiply the GI by the number of carbohydrates in the serving size and divide the result by 100, accounting for how starchy a particular food type is compared to others.
If a food has a low GI but a high proportion of carbohydrates, the GL will “correct” the value upwards to account for the food's high overall sugar load. Most foods will have similar GI and GL values, at least relative to other foods, as starchy foods tend to be digested quickly. Some people prefer the GL for this reason, as it adds an extra step to try to make sure nothing is missed.
After all, you can always choose to be informed by both values. GLs of over 20 are considered high, those 10 or under are considered low, and those from 11 to 19 are considered moderate.

How to use glycemic index charts
Since it’s exceedingly rare to find a person who eats 50 grams of pure glucose, we’ll take the common step of setting white bread as the baseline value. So, for this chart, when you see a GI of 25, for example, it means there will be a quarter as much glucose rise over the first two hours of digestion as with white bread.
CGM insights
Along with the other limitations of the GI mentioned above, this is one reason we consider it a good starting point, but by no means the end of the journey towards discovering which foods work best for you. A glucose biosensor or continuous glucose monitor (CGM) shows you how your meals affect your body 24/7. So there’s no guessing, just clarity. This device measures interstitial fluid in your arm to estimate glucose levels over a set period, usually 10 days or 2 weeks.
Eating speed
You can even see how a specific food works for you relative to the sample population from which the GI is derived by comparing your glucose results of the first two hours after eating the food to the reported GI. Even simple adjustments, like eating more slowly or swapping a side, can change your glucose curve more than you might expect.
Glycemic index charts for everyday foods
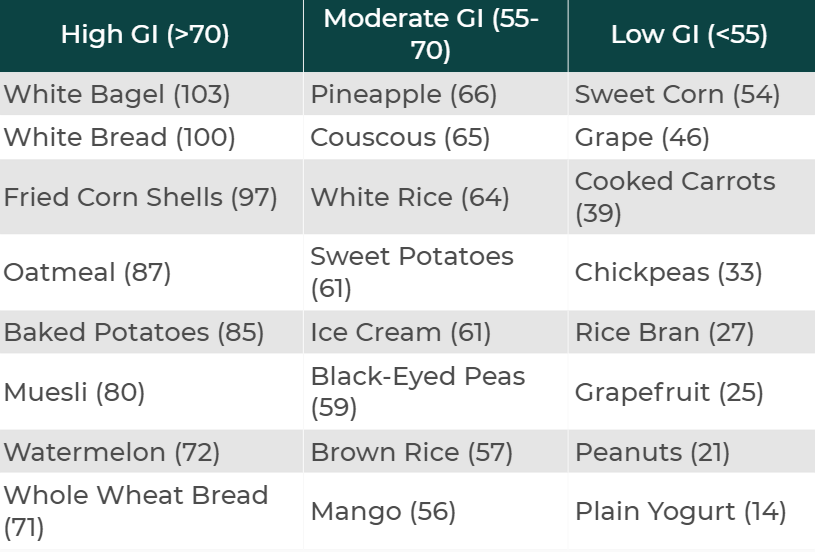
Which foods have a high Glycemic Index (GI)
- White Bagels: These have a GI of over 100 because we use white bread as the reference point; anything with a stronger glucose response than white bread will have a value over 100.
- Watermelon: It may be surprising to see fruit on this list, but watermelon is full of bioavailable sugars that are metabolized quickly.
Which foods have a moderate Glycemic Index (GI)
- Brown Rice: Whole-food starches tend to fall right in the middle of the GI distribution for all foods.
- Ice Cream: Although full of sugar and fat, ice cream takes a relatively long time to metabolize compared to starchy foods and fruits.
Which foods have a low Glycemic Index (GI)
- Plain Yogurt: One of our favorite foods to recommend due to its low GI and other positive health attributes.
- Grapefruit: The sweet and sour fruit has a surprisingly manageable effect on glucose levels up to two hours after eating.
When "Healthy" choices don't feel right
You’re at the grocery store, determined to stock up on healthy snacks for the week. You reach for a container of pre-cut watermelon, thinking it’s a perfect choice, it's fruit, after all. But then you pause, remembering that familiar energy crash you often get mid-afternoon, even on days you eat light.
You’re doing everything “right,” yet your energy, cravings, and progress still don’t align. This is where understanding the glycemic index comes in. That watermelon, while nutritious, has a high GI of over 70, which can cause a rapid rise and fall in your glucose. Knowing this helps you see that it’s not about willpower but about how your unique body responds to different types of food.
How does Nutrisense support low-glycemic eating
Your glucose quietly shapes how you feel throughout the day. But seeing the number alone isn’t enough. Nutrisense helps you interpret what it means, so you can eat in a way that supports energy, focus, and balance.
Dietitian guidance
Sign up to access insurance-covered video calls with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Program and app
With the Nutrisense Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Get started
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
Glycemic Index (GI) FAQ
Q1. How can I use a companion app like the Nutrisense App to review a 2-hour response after a meal?
A1. While this may change depending on the app you use, here’s a quick guide. Log your meal with portion details and time. Keep your routine steady for the next 2 hours to reduce confounders. Your biosensor measures glucose in interstitial fluid, and the app visualizes your curve so you can compare similar meals or preparation methods. Add notes and tags to track pairings or meal orders for later review.
Source: Nutrisense App: How To
Q2. Does Nutrisense include glycemic index or load values in the app?
A2. The app focuses on your own patterns rather than preset GI or GL values. You can log foods, portion sizes, and preparation details, then compare your 2-hour curves to see how different choices affect you. Your dietitian can help you translate these patterns into practical swaps that fit your day.
Source: Nutrisense App: How To
Q3. What exactly does the Nutrisense biosensor measure?
A3. The sensor tracks glucose measured in interstitial fluid. Data flows to the Nutrisense app, allowing you to see patterns across meals, movement, and sleep. This helps you test meal orders, pairings, and portions using your own responses, then discuss options with a registered dietitian to support sustainable habit changes.
Source: How Nutrisense Works
Q4. Can I use Nutrisense if I already have my own sensor?
A4. Yes. You can subscribe to bring your own sensor and still use the Nutrisense app and coaching. This option allows you to connect your device, log meals and activities, and review your patterns with a dietitian. Check plan details on device compatibility and what is included before you enroll.
Source: Bring Your Own Sensor
Q5. Are dietitian video calls available, and how do they work with low glycemic goals?
A5. Members can book 1:1 video calls with a registered dietitian. Sessions focus on your data, preferences, and schedule to refine meal order, pairings, and portions. Many plans are covered by insurance, but coverage varies by plan. Review eligibility details and booking steps on the program page.
Source: Nutritionist Video Calls
Methods & Sources
This page summarizes how glycemic index/load relate to glucose responses and outlines Nutrisense’s data‑guided approach; methods and citations are listed below.
Methods:
- Weight Loss Report
- Personalized Guidance Outcomes
- Subjective Well-Being Survey
- Nutrisense Weight Outcomes
- How Nutrisense Works
Peer-reviewed References:
- Glycemic Goals and Hypoglycemia: Standards of Care in Diabetes—2024 — Diabetes Care (2024). DOI/PMID: https://doi.org/10.2337/dc24-S006
- Diabetes Technology: Standards of Care in Diabetes—2024 — Diabetes Care (2024). DOI/PMID: https://doi.org/10.2337/dc24-S007
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Kara Collier is a registered dietitian nutritionist and certified nutrition support clinician who is passionate about reshaping how we approach prevention, behavior change, and metabolic health. A Forbes 30 Under 30 honoree, she’s helped over 150,000 people improve their metabolic health using tools like continuous glucose monitors and behavior-focused nutrition strategies. Kara has been featured by Forbes, UC Berkeley, and HLTH, and has appeared on top podcasts like Mind Pump and The Genius Life.




