Normal Blood Glucose Levels: What They Are and How to Monitor Them

Key Takeaways
Everyone’s talking about blood glucose levels (or blood sugar levels), but do you know enough about what they are and why they’re important to pay attention to? And even with all the information available, do you know what “normal” means when it comes to blood sugar levels?
If not, don’t worry. It can be challenging to sift through all the information out there to figure out how to learn more about yours. Luckily, we’re here to help!
First, you should know that glucose is the main sugar found in your blood. It’s a simple carbohydrate that’s your body's primary energy source and it comes from many foods, such as bread, fruits, and vegetables. A target range for blood glucose levels is important because the amount of glucose in your blood changes throughout the day.
So, what’s the normal range for blood sugar? Here’s what you need to know about blood sugar ranges, and what normal blood glucose levels look like.
What is Blood Glucose?
Learn more about how your body uses glucose with the Nutrisense Program—take our quiz here.
Glucose is a simple sugar—the most basic of all carbohydrates. Blood sugar, or blood glucose, is the sugar that circulates in your bloodstream and provides your body with energy.
Your body constantly regulates your blood sugar levels to keep them within the normal range outlined by the CDC. Glucose levels, in particular, are regulated by a hormone called insulin, released from the pancreas. While insulin may be able to help reduce blood sugar levels, hormones like glucagon and cortisol can raise blood sugar.
When your blood glucose levels are too high, your body releases insulin to bring them back down. When your blood glucose levels are low, your body releases glucagon to raise them.
Here’s a fun fact: the average person has about one teaspoon of sugar in their bloodstream at any given time. If your blood sugar levels rise too far above or below that one teaspoon, your pancreas releases hormones to keep the balance.
When you have too much sugar in your blood, it leads to elevated blood glucose levels, also known as hyperglycemia. A high-carb or sugar-heavy meal can lead to instances of postprandial hyperglycemia.
Chronic hyperglycemia can also be one of the signs of diabetes. Symptoms often include things like excessive thirst, fatigue, and blurred vision. In some cases, chronic hyperglycemia may be a cause of diabetes complications like diabetic ketoacidosis if it is left unaddressed.
How is Blood Glucose Measured?
Glucose levels are measured in mg/dL, or milligrams per deciliter. This measures the concentration of a substance in a specific amount of fluid, or the concentration of glucose in your bloodstream.
You may also see a less common measurement: mmol/L, or millimoles per liter. If you ever need to make sense of that one, remember that mg/dL is mmol/L multiplied by 18. You can also use our blood sugar conversion chart to make it even easier to understand your levels in either measurement.
{{rich-text-cta-2="/style-guide"}}
What are Normal Blood Glucose Levels for People without Diabetes?
According to researchers, the range for normal glucose levels is typically between 70-100 mg/dL when fasting, and maximum post-meal levels of less than 140 mg/dL (two hours after eating). However, normal blood glucose levels vary from person to person and depend on various factors.
It’s important to note that there is no one-size-fits-all answer to this question. But, if your blood sugar levels consistently fall outside of this range, it could be a sign that you need to speak with your doctor.
For those who don’t have diabetes, normal levels can also vary according to whether you have a healthy diet and lifestyle factors like sleep hygiene and blood pressure. Typical blood glucose levels can also vary depending on age, weight, and activity level. You can use a CGM without diabetes to get a better understanding of how your own glucose levels fluctuate.
Stress, illness, some medical conditions, and even certain medications can also affect your blood sugar levels—everything from a heart attack to a new weight loss goal can impact them. So if you're wondering what normal blood glucose levels look like for you, it's best to talk to a healthcare provider.
Here are some general guidelines for normal blood sugar levels.
Normal Fasting Blood Sugar Levels
A “fast” is when you go without food for an extended period of time, and drink only water. Most people fast throughout a night of sleep and break their fast first thing in the morning after eight hours of rest. This is why fasting blood glucose levels are usually recorded just before breakfast.
The American Diabetes Association (ADA) describes average fasting blood glucose as anything under 100 mg/dL. The World Health Organization (WHO) provides a similar normal fasting range of 70-100 mg/dL.
But a fasting blood glucose level near 100 mg/dL isn’t always ideal. Research shows that people with fasting blood glucose levels consistently between 91-99 mg/dL are more likely to develop diabetes.
The ADA recommends seeing your healthcare provider if you get two consecutive readings above 100 or below 70 mg/dL.
Blood Sugar Levels Two Hours After Eating
It’s also important to know how your body responds to the foods you eat. Glucose is a simple carbohydrate, so the carbs in your diet like bread, beer, and potatoes may cause higher spikes in your blood glucose.
Balancing your meals with protein and fiber-filled foods is a great way to blunt a higher glucose spike and keep your levels stable. It can also be an excellent way to meet your nutrient needs!
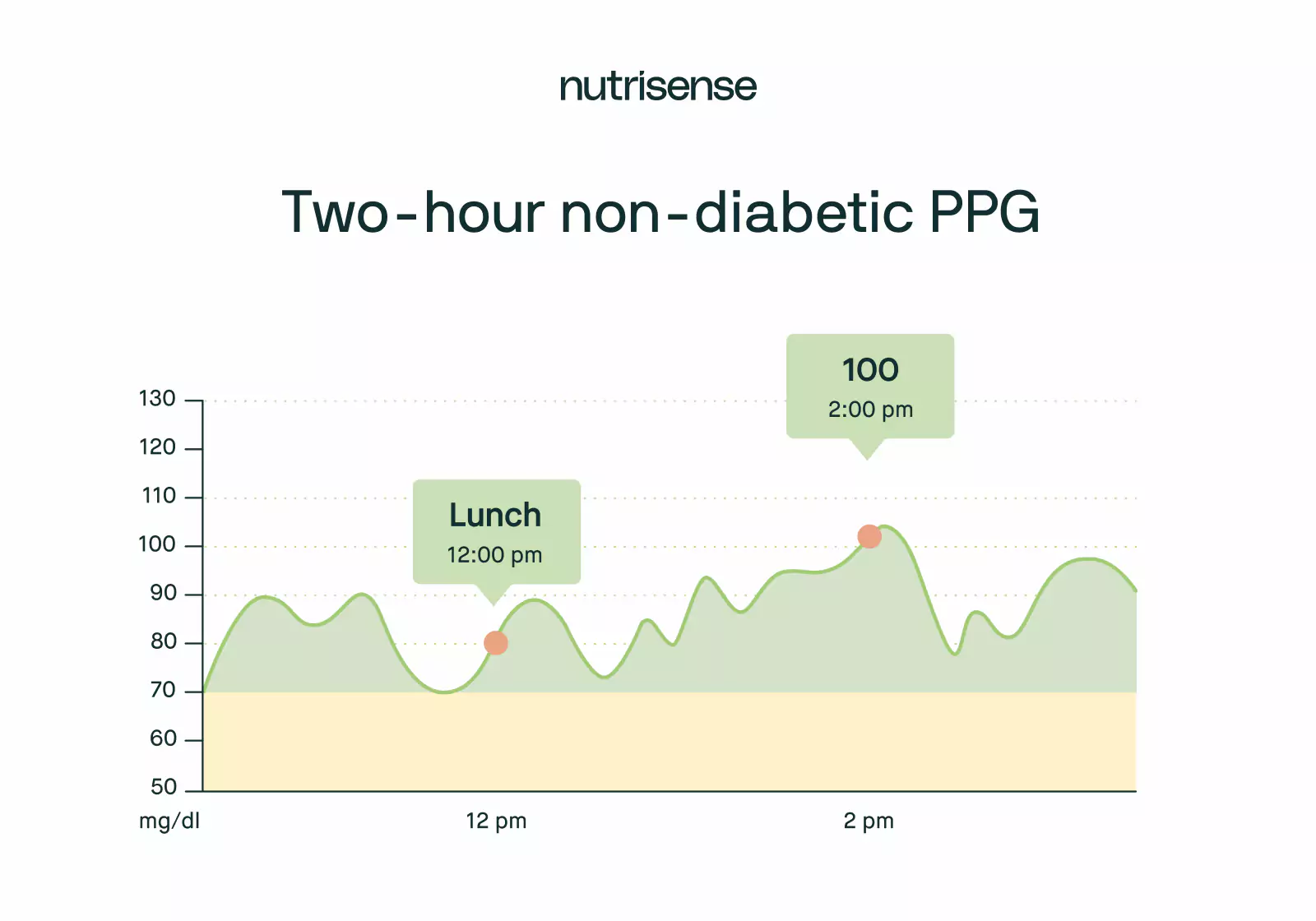
The scientific term for this post-meal glucose test is a postprandial glucose test (PPG). For those without diabetes, a two-hour postprandial glucose test should ideally show blood sugar levels between 70-140 mg/dL according to the ADA.
Normal Maximum or Peak Glucose Levels
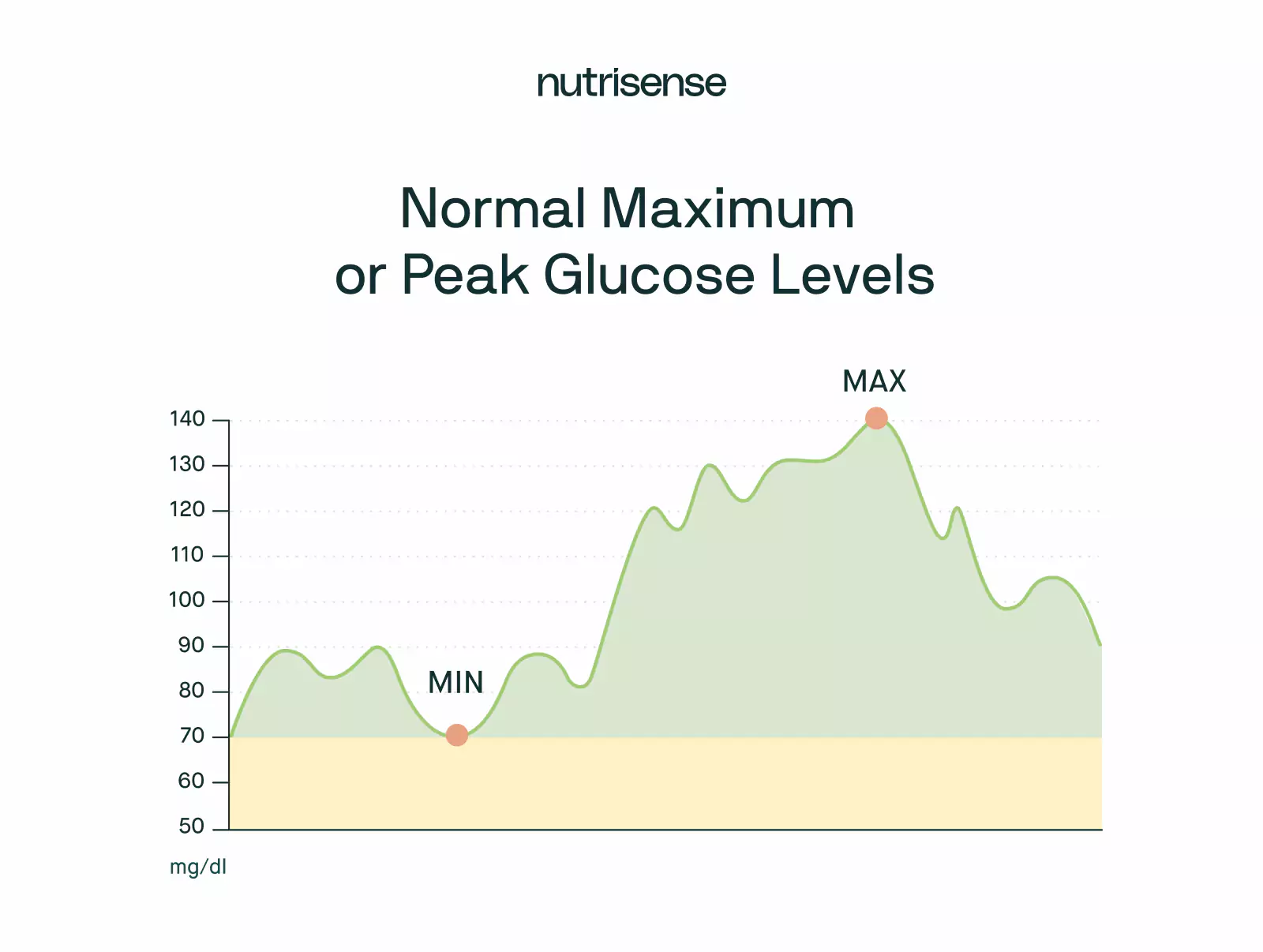
Eating provides your body with the energy it needs throughout the day. So, it’s not surprising that your blood glucose levels spike after a meal.
According to the ADA, readings directly after a meal should be below 140 mg/dL for a healthy adult. Remember, keeping your blood sugar levels below this threshold may also help minimize some risk factors for medical conditions like prediabetes.
Regardless of mitigating factors like eating patterns, any two tests (taken two hours apart) that show blood sugar levels over 140 mg/dL can be concerning. And, if you have readings over 200 mg/dL, it’s a good idea to get in touch with your healthcare provider.
Determining Normal Average Blood Glucose Levels for Non-Diabetics
Most people know that if you have diabetes, you may need to keep track of your blood sugar levels. This may be helpful for people without diabetes too, and the good news is that it doesn’t have to be complicated. Non-diabetic glucose monitoring using a CGM is one way to do this.
The key takeaway to remember is that while blood sugar levels vary, a good starting point is maintaining a normal fasting range of 70-100 mg/dL.
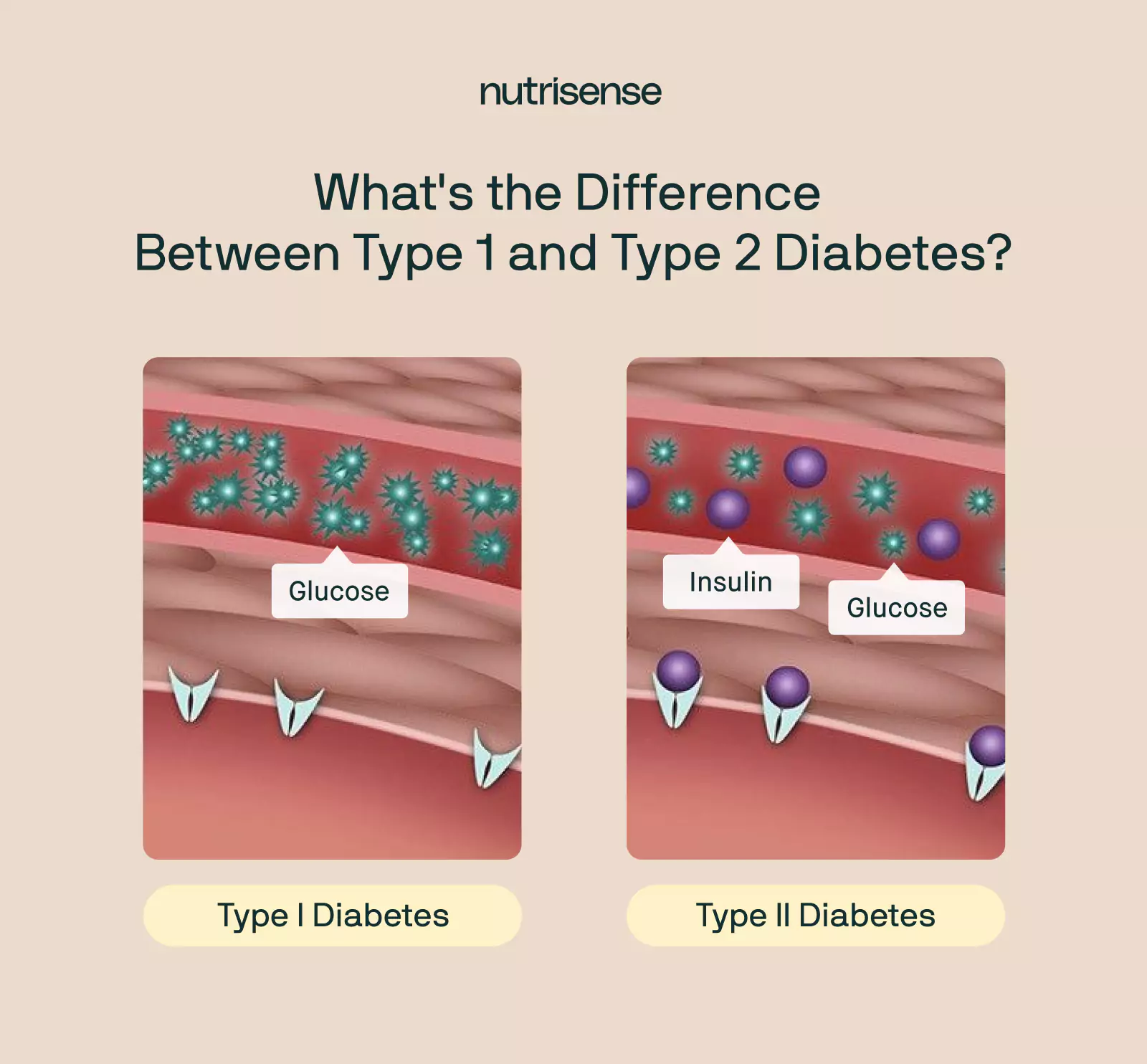
What are Normal Blood Glucose Levels for People with Diabetes?
Diabetes, known medically as diabetes mellitus, is a group of disorders related to an abundance of glucose in the blood. For people with diabetes, the CDC recommends fasting blood sugar levels between 80 and 130 mg/dL—although the ideal fasting blood glucose is around 110 mg/dL.
While it may be a good idea for everyone to optimize their blood glucose levels, it’s often necessary for people with diabetes. If your body cannot produce enough insulin, your healthcare provider may consider further testing for type 1 diabetes. Type 2 diabetes, on the other hand, occurs when your body cannot properly regulate and use blood glucose due to issues like insulin resistance.
The average blood sugar levels for those living with diabetes are slightly different from those without diabetes. And pregnant women who may develop gestational diabetes have different ranges too. Individual factors such as age and medical history may also change what an average level looks like for you.
It’s always best to find your ideal range from a doctor, but if you’re curious about what normal blood glucose levels look like for those with diabetes, read on!
Fasting Blood Glucose Levels
Proper treatment for diabetes can require regular testing. For many people with diabetes, that means taking a fasting blood glucose test before breakfast. As we mentioned above, a range between 80 and 130 mg/dL for fasting blood sugar levels is recommended by the CDC for people with diabetes.
Two-Hour Postprandial Blood Glucose Levels
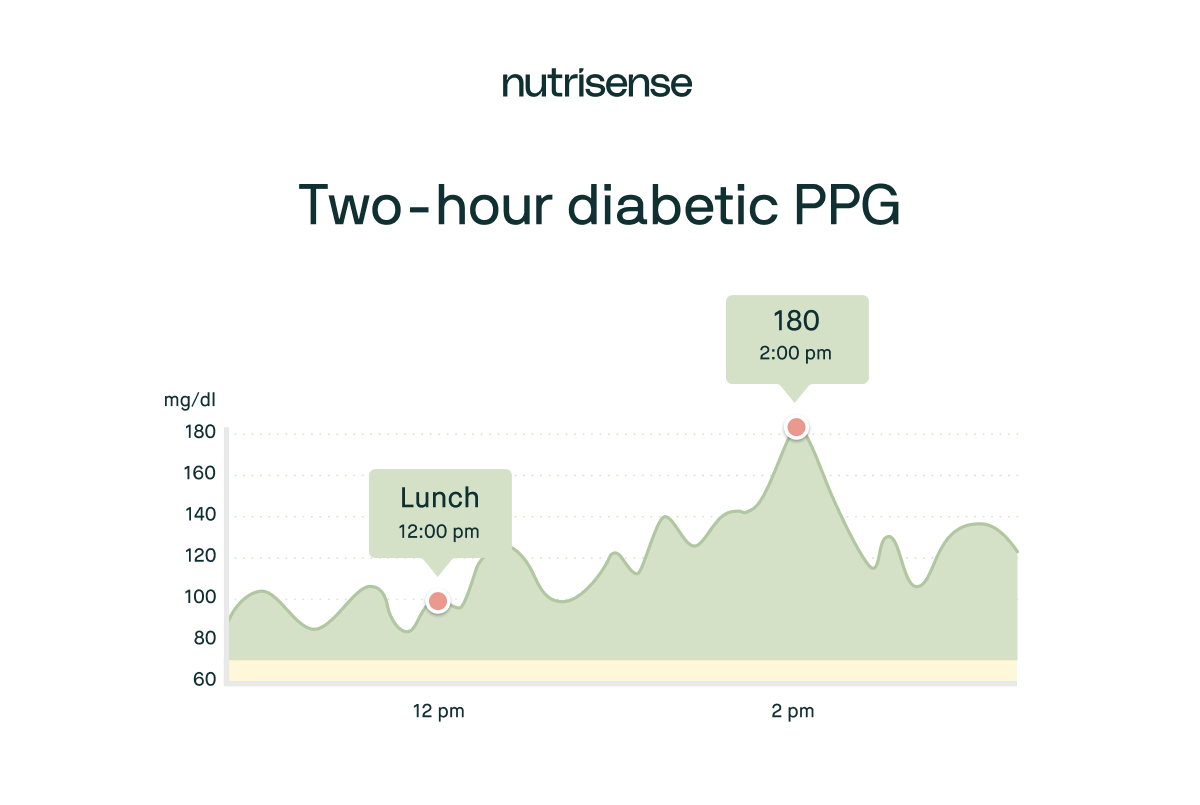
The two-hour PPG test is another benchmark for those with diabetes. The CDC suggests aiming for a two-hour PPG below 180 mg/dL. However, for a healthy lifestyle, at or below 140 mg/dL considered by the CDC to be ideal.
Peak Glucose Value
With or without diabetes, blood glucose levels usually peak around 30-60 minutes after eating. Readings over 240 mg/dL can be dangerous, so it’s best to consult a doctor if you see those.
A1C or Average Glucose Readings
The glycated hemoglobin, or A1C test, is a medical blood test result used to gauge how much glucose has been in a person’s blood over a three month period. It reflects an average of the ups and downs of blood glucose levels over a longer time.
Most people with diabetes are advised by the CDC to take an A1C test at least twice a year and aim for levels below seven percent.
A1C test results are also known as Estimated Average Glucose (eAG) tests, and you can use eAG to calculate an estimation of your A1C percentage. An A1C level of seven percent correlates to an eAG of 154 mg/dL.
A Note on Hypoglycemia and Diabetes
With all the talk of high blood sugar, it’s easy to forget that low blood sugar can also be an issue—especially for people with type 1 or type 2 diabetes. Too much insulin can lead to hypoglycemia or unhealthily low blood sugar levels.
For those with diabetes, blood sugar levels below 70 mg/dL are hypoglycemic levels. Some of the symptoms of hypoglycemia may include:
- Sweating
- Tingles
- A racing heartbeat
- Mood changes
- Dizziness
- Confusion
Learn more about very low blood sugar levels (hypoglycemia) and high blood sugar levels (hyperglycemia) here.
Find the right Nutrisense programto turn insight into progress.
Are My Blood Glucose Levels Normal?
As we’ve mentioned throughout this article, normal blood sugar levels can vary depending on various factors. However, the guidelines and resources in this article can help you determine if you’re within a healthy target range.
If you're still confused by all the numbers, here's a handy list of blood sugar charts by age that may help. And if you're struggling with unstable blood glucose levels or want a deeper understanding of your body’s metabolic health, try the following tools.
Glucometer
A glucometer is a small, portable device with which you can measure the sugar level in your blood. Small, portable, and easy-to-use, it involves pricking your finger, touching a drop of blood to the test strip, and letting the machine do the rest!
The most obvious drawback is the finger prick. Glucometers, or glucose meters, also need a constant supply of testing strips, and while some come equipped with onboard memory, most do not. You'd need to keep a journal to write down the time of each test and the corresponding blood sugar level.
Continuous Glucose Monitors or Glucose Biosensors
By contrast, one of the benefits of a CGM or glucose biosensor is that it continuously measures and records your glucose levels. These devices actually measure interstitial glucose, and do this through a sensor placed on the skin, usually on the “fatty” part of your upper arm.
A small filament is inserted under the skin to measure your glucose 24/7, which makes CGMs a good option for those looking to understand their blood glucose trends. However, to make the most of your data, you need expert support, like from a registered dietitian or nutritionist trained to work with glucose data.
Hemoglobin A1C Test
The A1C hemoglobin test is a physician-ordered blood sugar test that involves a blood sample. A normal A1C level is below 5.7 percent, a level of 5.7 to 6.4 percent indicates a risk for prediabetes, and a level of 6.5 percent or more is a sign of diabetes.
There may be some concerns over the accuracy of the A1C test for some people and some cases. For more information, here’s a user-friendly guide to A1C.
Fructosamine
Fructosamine is a compound produced in the body when glucose combines with protein. Like A1C hemoglobin, measuring fructosamine levels may provide another stable benchmark.
Because fructosamine testing does not rely on hemoglobin, it can provide more accurate results for those with atypical blood cells.
Oral Glucose Tolerance Test
The oral glucose tolerance test is a doctor-prescribed test that gauges how your body reacts to an influx of glucose. They are a standard test during pregnancy to check for gestational diabetes.
The test begins with a blood draw to determine a baseline blood sugar level. Then, the patient drinks eight ounces of liquid glucose—usually a total of 75 grams of carbohydrates. After a few hours, the test requires another blood draw to see how your body handles the influx of glucose.
Some researchers argue that a one-hour post-meal test is superior to the standard 2-hour PG test and may be more adequate to identify high-risk individuals. As the data is reviewed more deeply, the 1-hour PG levels could eventually replace the 2-h OGTT as the standard.
Find Your Normal Glucose Level Range with Expert Guidance
Remember, normal glucose levels are not always the same for everyone. To find out what ‘normal’ looks like for you, it’s a good idea to keep a pulse on your unique blood glucose levels in relation to your health and lifestyle. They’re affected by everything from stress and sleep to food and exercise too!
Using a tool like a CGM sensor or glucose biosensor is a helpful way to see your levels, but it's just the beginning. To make the most of the data, you need to know how to interpret it, and that’s where you need expert guidance from a glucose expert like Nutrisense’s registered dietitians and nutritionists. Using your CGM or glucose biosensor with a program like Nutrisense gives you the support, advice, and tools to turn this data into an actionable health plan.
Nutrisense gives you access to glucose biosensors, or you can also bring your own continuous glucose monitors (CGMs) to use with the program. And the best part, is that you can sign up for 1:1 support from a board-certified, registered dietitian through options like insurance-covered video calls. You can work with a glucose expert whose specialties align with your health goals and needs to determine what normal glucose levels look like for your unique body.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Heather is a Registered and Licensed Dietitian Nutritionist (RDN, LDN), subject matter expert, and technical writer, with a master's degree in nutrition science from Bastyr University. She has a specialty in neuroendocrinology and has been working in the field of nutrition—including nutrition research, education, medical writing, and clinical integrative and functional nutrition—for over 15 years.




