What is a Normal Glucose Level Chart: A Guide by Age

Key Takeaways
Even if you know the typical ranges for normal glucose levels, you may still be wondering if your age factors in here. And it might!
Since knowing your blood sugar levels are an important way to keep track of your glucose, and overall wellness, it’s a good idea to understand more about them. And as it turns out, these sugar, or blood glucose levels, can vary for many reasons, including your age. They can also vary among different age groups and at different times of the day. It can be challenging to figure all this out on your own.
This guide breaks down normal fasting and post-meal glucose levels by age group with some handy blood sugar level charts included—and offers some practical tips and warning signs to watch for.
What’s a Normal Blood Sugar Level?

Before we start talking about the numbers, remember: a "normal" blood sugar level” varies based on many factors. A good way to learn more about your levels is to consult with a qualified healthcare professional. But first, here’s a quick reminder of what blood sugar is from a diabetes educator and glucose expert:
"Your body breaks down carbohydrates into glucose, which is your body’s primary energy source. The pancreas then releases insulin to shuttle glucose into your cells, where it’s converted to energy. Glucose may also be stored as glycogen in your liver and muscles or as fat in adipose tissue. Insulin and glucagon, along with other hormones, help regulate the amount of glucose in your bloodstream." — Kara Collier RDN, LDN, CNSC
To read more about how the body regulates glucose balance, check out our article on glucose homeostasis. Remember, it’s normal for glucose levels to fluctuate to some degree. Blood sugar levels are influenced by many factors, including:
- The type and quantity of food you consume and when you consume it
- The amount and intensity of the physical activity you engage in
- Any medications you may be taking
- Medical conditions, health conditions (like cholesterol) and chronic illnesses you may have
- Your age
- The amount of stress you experience
- Dehydration
- Hormones, including sex hormones and menstrual cycle timing
- Certain herbs or bioactive compounds, including caffeine
- Alcohol consumption
Typical glucose values are often listed as a range to help capture any normal fluctuations that may occur within that range. Additionally, for those who may have health conditions like prediabetes or diabetes (characterized by some level of insulin resistance), a normal glucose range may be broader or more lenient.
Now let’s dive into some specifics on normal levels based on different age ranges!
{{rich-text-cta-2="/style-guide"}}
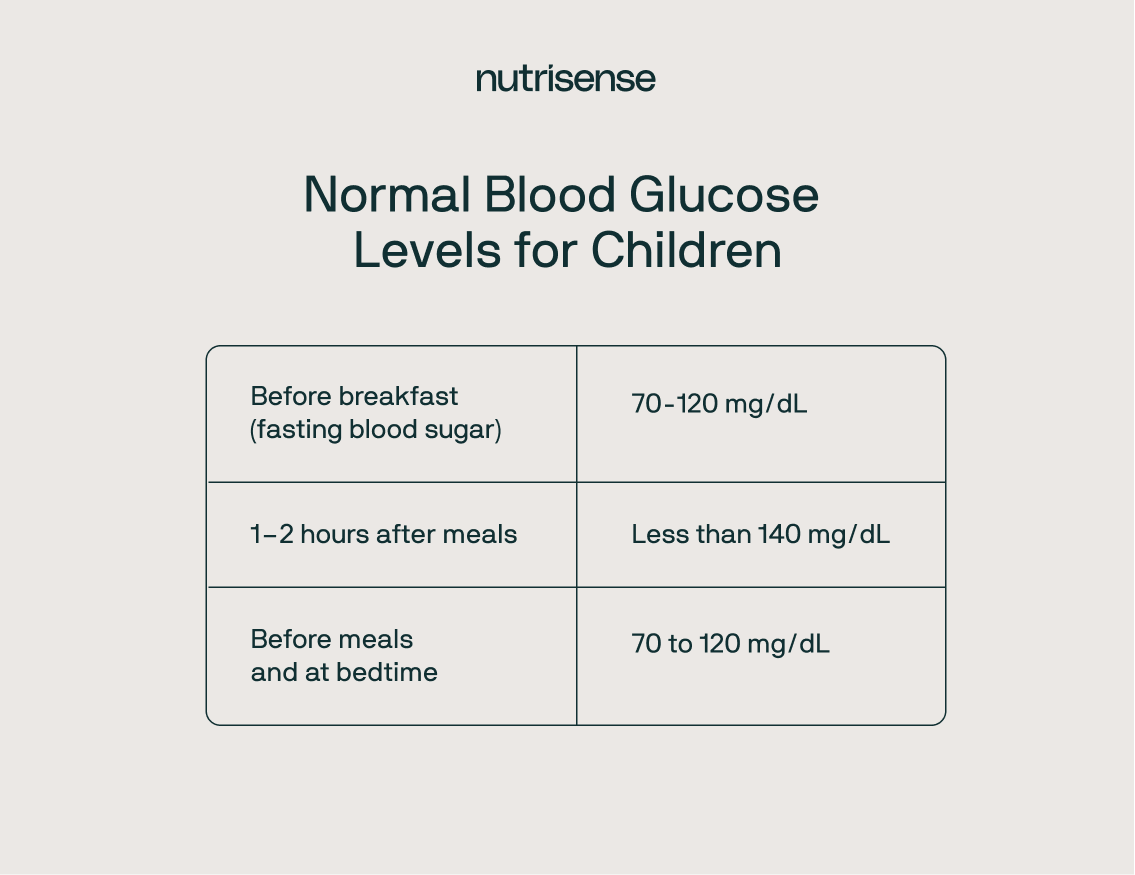
Normal Blood Sugar Levels Chart for Children [Ages 6-12]

According to Nationwide Children’s Hospital, children without diabetes between the ages of 6-12 should have normal glucose readings that look like this:
- Before breakfast (fasting blood sugar): 70 to 120 mg/dL
- One to two hours after meals: Less than 140 mg/dL
- Before meals and at bedtime: 70 to 120 mg/dL
Children without diabetes don’t typically need regular blood sugar checks (unless they have a have a medical condition like type 1 diabetes), but knowing healthy ranges can help parents notice potential concerns.
For children with diabetes, the amount of glucose in the blood will fluctuate from when they wake up, based on their activity levels, and before they sleep at night.
Despite all this, recommendations suggest blood glucose levels should stay between 80-180 mg/dL throughout the day.
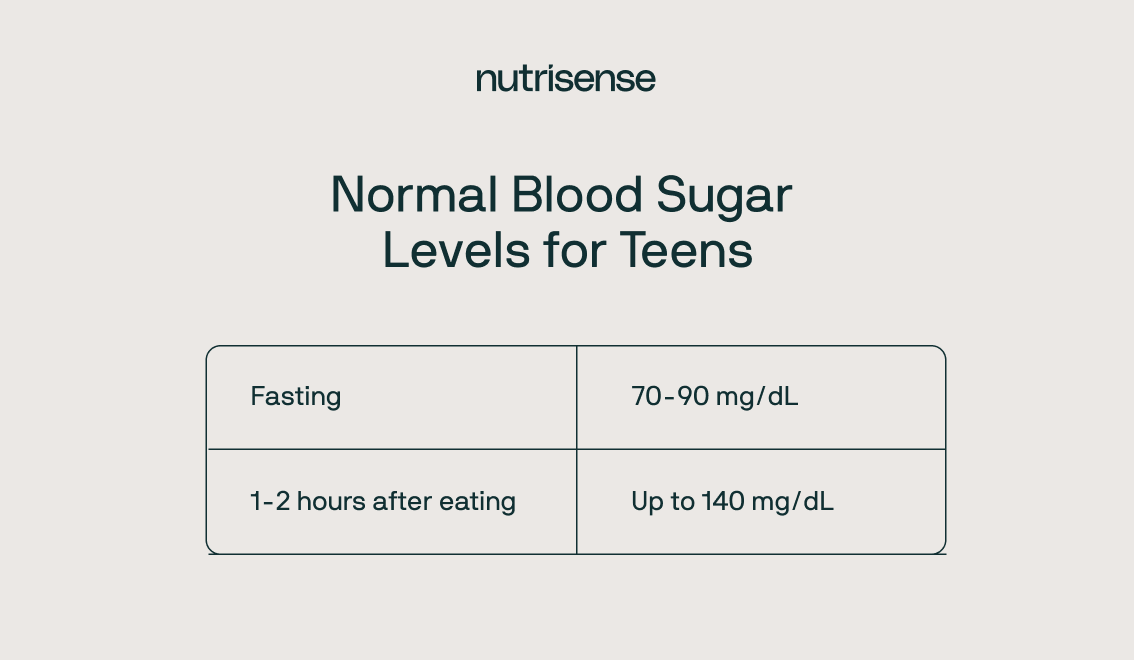
Normal Blood Sugar Levels Chart for Teens [Ages 13-19]

- Fasting: 70–140 mg/dL
- Post-meal: <140 mg/dL
There are no set guidelines by the American Diabetes Association for typical blood glucose for teens without diabetes. The Mayo Clinic recommends aiming for the same guidelines for healthy children/adults without diabetes, keeping glucose between 70-140 mg/dL.
For teenagers with diabetes, it’s a good idea to consult with your doctor for specific guidance. Some research on teens with type 1 diabetes recommends aiming for blood glucose levels between 70-150 mg/dL throughout the day.
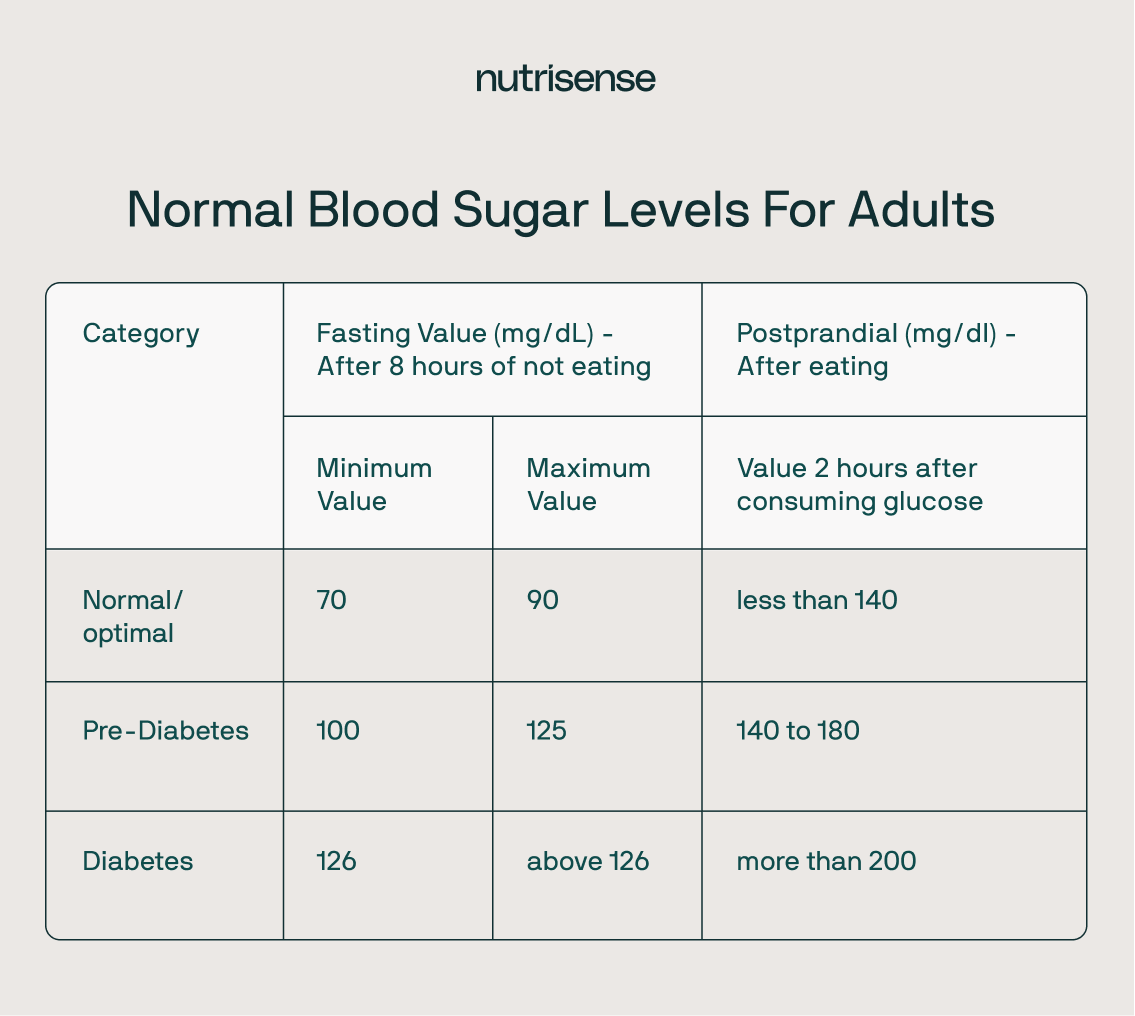
Normal Blood Sugar Levels Chart for Adults [Ages 20+]
- Optimal fasting: 70–90 mg/dL
- Post-meal: <140 mg/dL
The majority of the research on normal glucose levels has focused on adults. While you may notice that different labs may have distinct reference ranges, studies show that optimal fasting glucose for minimizing risk for prediabetes may be between 70-90 mg/dL for adults without diabetes.
Research also shows that fasting glucose levels above 90 can lead to an increased risk of cardiovascular disease.
Factors that Impact Higher Fasting Blood Sugar Levels
There are many factors that can impact a higher fasting blood glucose value. It’s essential to pay attention to things like:
- What and when you ate the night before
- Sleep quality and quantity
- Stress levels
It may also be helpful to monitor your alcohol intake, note any supplements you’re taking, and monitor your overall physical activity and body weight. Working 1:1 with a qualified healthcare professional, including a credentialed, registered dietitian or nutritionist, can help you make sense of some of these patterns and how they can affect your overall well being.
Here’s some more interesting facts about glucose level charts:
- The expected glucose ranges for adults with diabetes will differ from the target ranges for adults without diabetes.
- The American Diabetes Association also suggests different glucose ranges for healthy adults, adults with prediabetes, and adults with diabetes.
- Healthy adults without diabetes should keep glucose between 70-140 mg/dL.
- According to the International Diabetes Federation (IDF) guidelines, adults with healthy glucose metabolism should stay below 140 mg/dL after meals.
- Healthy adults have been shown to remain below 140 mg/dL, 95-99 percent of the time.
- Most healthy people will see a peak glucose value within 30 minutes of eating.
- Spikes above 160 mg/dL may be problematic. Monitoring glucose can help you assess your risk for conditions like prediabetes and diabetes.
How is Prediabetes Linked to Glucose Fluctuations?
Wondering where prediabetes and diabetes factor into all of this? Here’s some quick information:
- The ADA classifies prediabetes fasting glucose levels above 100 mg/dL and up to 125 mg/dL and a two-hour postprandial level between 140-199 mg/dL. It’s usually diagnosed with a blood sugar test called an oral glucose tolerance test.
- An A1C between 5.7-6.4 percent is considered a prediabetic level by the ADA.
- Diabetes is typically diagnosed after two repeat fasting glucose tests above 125 mg/dL or a two-hour reading above 200 mg/dL after an oral glucose tolerance test.
- Additionally, an A1C above 6.5 percent is considered a diabetic level by the ADA.
- Diabetes may also be diagnosed if a random blood sugar check at any time of the day is above 200 mg/dL.
Normal Blood Sugar Levels Chart for Older Adults [ Ages 65+]

- Fasting: 70–140 mg/dL
- Post-meal: <160 mg/dL (may vary)
Let’s spend a minute discussing the average levels for adults over the age of 65. Those who do not have diabetes may be held to the same glucose range as healthy younger adults, keeping glucose between 70-140 mg/dL during the day.
For older adults with diabetes and co-morbidities or severe diabetes symptoms like neuropathy, kidney damage, or retinopathy, the recommended glucose threshold, and A1C values may be more lenient. It will all depend on how much damage is done to the pancreas.

Warning Signs of High Blood Sugar

While there are ways to track, monitor, and determine whether you have high blood sugar levels, you may not always know when you’re experiencing it. Often, there are no warning signs until your levels rise much higher than the expected range.
For example, adults with prediabetes may not realize they have this condition based on symptoms alone. However, here are some classic symptoms of high blood sugar that may occur:
- Fatigue
- Frequent urination
- Headaches
- Blurred vision
- Difficulty concentrating/ Brain fog
- Increased thirst
- Anxiety
- Increased cravings
Track and Monitor Your Glucose with Health Tech
It’s easy to attribute these symptoms to other causes, some as seemingly routine as feeling thirsty or getting a slight headache! That’s where using health tech, including wearables like glucose biosensors or continuous glucose monitors (CGMs)—which check interstitial glucose but can give you a good indication of your average blood sugar over time—can be invaluable.
How To Lower Blood Sugar

There are many ways to address higher glucose readings that are practical and can be done each day.
Here are a few tips for some lifestyle changes that may help from Nutritionist Liz McKinney, MS, CNS, LDN:
- Get some exercise. Exercise isn’t just good for weight loss, it’s a great way to boost your overall wellness! It may also help support healthy blood sugar levels. Even just a post-meal walk, or aiming for 10,000 steps daily can help.
- Drink some apple cider vinegar in some water before your meals. Meta-analyses suggest that ingesting vinegar at the start of a meal—one to two tablespoons in a glass of water—can diminish the post-meal (or “postprandial”) surge in blood glucose. For two hours after a meal, vinegar consumption is associated with a reduction in postprandial blood sugar of about 20 to 40 percent.
- Focus on protein-rich meals. While everyone will have a different protein target, aiming to eat adequate protein at each meal helps to produce a gentler glucose curve and may improve glucose response.
- Avoid eating late at night. Studies show that this may lead to higher post-meal glucose spikes—even in healthy, non-diabetic individuals.
- Work on stress management. Easier said than done, we know! But stress can be one of the risk factors for high blood sugar. When your body is stressed, it releases cortisol, which tells your liver to release glucose into your bloodstream as a quick energy source. Here are a few great tips to help you relieve stress.
Warning Signs of Low Blood Sugar

Blood glucose monitoring isn’t just about learning more about high blood glucose levels. There’s also the chance they’ll dip! When blood glucose levels drop below 70 mg/dL, it’s known as hypoglycemia.
Some common symptoms of hypoglycemia include:
- Lightheadedness
- Dizziness
- Confusion
- Irritability
- Shakiness
- Nervousness/Anxiety
- Chills
- Sweating/Feeling clammy
- Rapid heart rate
- Pale skin
- Hunger
- Sleepiness
Find the right Nutrisense programto turn insight into progress.
How to Raise Your Blood Sugar
When blood sugar drops <70, accompanied by any of the common symptoms we’ve mentioned so far, it may be necessary to work on raising it. One way to do this is to eat 15 grams of quickly absorbing carbs (like apple juice or a glucose tablet), then wait 15 minutes for blood glucose levels to rise.
Once your glucose returns to a normal range, it can help to eat a protein or fiber-focused meal to prevent future dips. Glucose-certified nutritionist Liz McKinney, MS, CNS, LDN has a helpful suggestion!
"I suggest unsweetened Greek yogurt with berries or one to two hard-boiled eggs with sliced avocado on a slice of whole-wheat toast, it's a great option to help in these situations."
If you eat a low carbohydrate diet, seeing your glucose dip <70 may not be a cause for concern. It’s because your body may already be accustomed to lower baseline glucose. In this case, it’s important to watch out for any symptoms and also speak with a doctor to determine parameters appropriate for your body.
Understand Your Glucose Levels with Nutrisense
Understanding your blood sugar levels in relation to your age and health goals will help maintain overall wellbeing. While you can ask a healthcare provider for a test, use glucose meters and check your A1C levels every few months, keeping a continual eye on it is your best best.
That's where signing up for a program like Nutrisense can be a game-changer. With Nutrisense’s CGM Program, you also get access to glucose biosensors, or you can connect any compatible CGM to the Nutrisense App. Of course, the data won’t tell you the whole story, so it’s best to consult a credentialed expert! Sign up for personal coaching with a registered dietitian or nutritionist, 1:1 via insurance-covered video calls. The team of experts is trained to work with your body’s data have various specialties, from weight loss and prediabetes to cholesterol, sports nutrition and women's health.
Ready to get started? Take our quiz to see how Nutrisense can help you achieve your health goals.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Kara Collier is a registered dietitian nutritionist and certified nutrition support clinician who is passionate about reshaping how we approach prevention, behavior change, and metabolic health. A Forbes 30 Under 30 honoree, she’s helped over 150,000 people improve their metabolic health using tools like continuous glucose monitors and behavior-focused nutrition strategies. Kara has been featured by Forbes, UC Berkeley, and HLTH, and has appeared on top podcasts like Mind Pump and The Genius Life.




