What is PCOS and How Does It Affect Glucose?

Key Takeaways
Did you know that insulin resistance affects 50 to 95 percent of women with polycystic ovary syndrome? PCOS is a condition that affects the way your body regulates hormones and other related processes, and can lead to unpleasant symptoms like weight gain, acne, and irregular periods.
In addition to the physical symptoms this condition can cause, PCOS is also associated with a higher risk of conditions like heart disease, type 2 diabetes, high blood pressure, and even stroke.
September is national polycystic ovary syndrome (PCOS) awareness month. In the spirit of raising awareness about this important health issue that affects millions of women, including celebrities like Victoria Beckham and Lea Michele, let’s take a look at this condition, its signs and symptoms, and how it can affect other areas of your well-being.
When the Clues Are More Than Skin-Deep
You notice the skin around your neck seems a little darker, a stubborn patch that won’t wash off. It’s another frustrating mystery, along with the persistent fatigue and the number on the scale that refuses to move, no matter how carefully you eat.
You’ve been told this can be part of having PCOS, but you need more than a label. You want to understand what’s actually happening inside your body so you can finally find a path that leads to real progress.
What Symptoms Are Associated with PCOS?
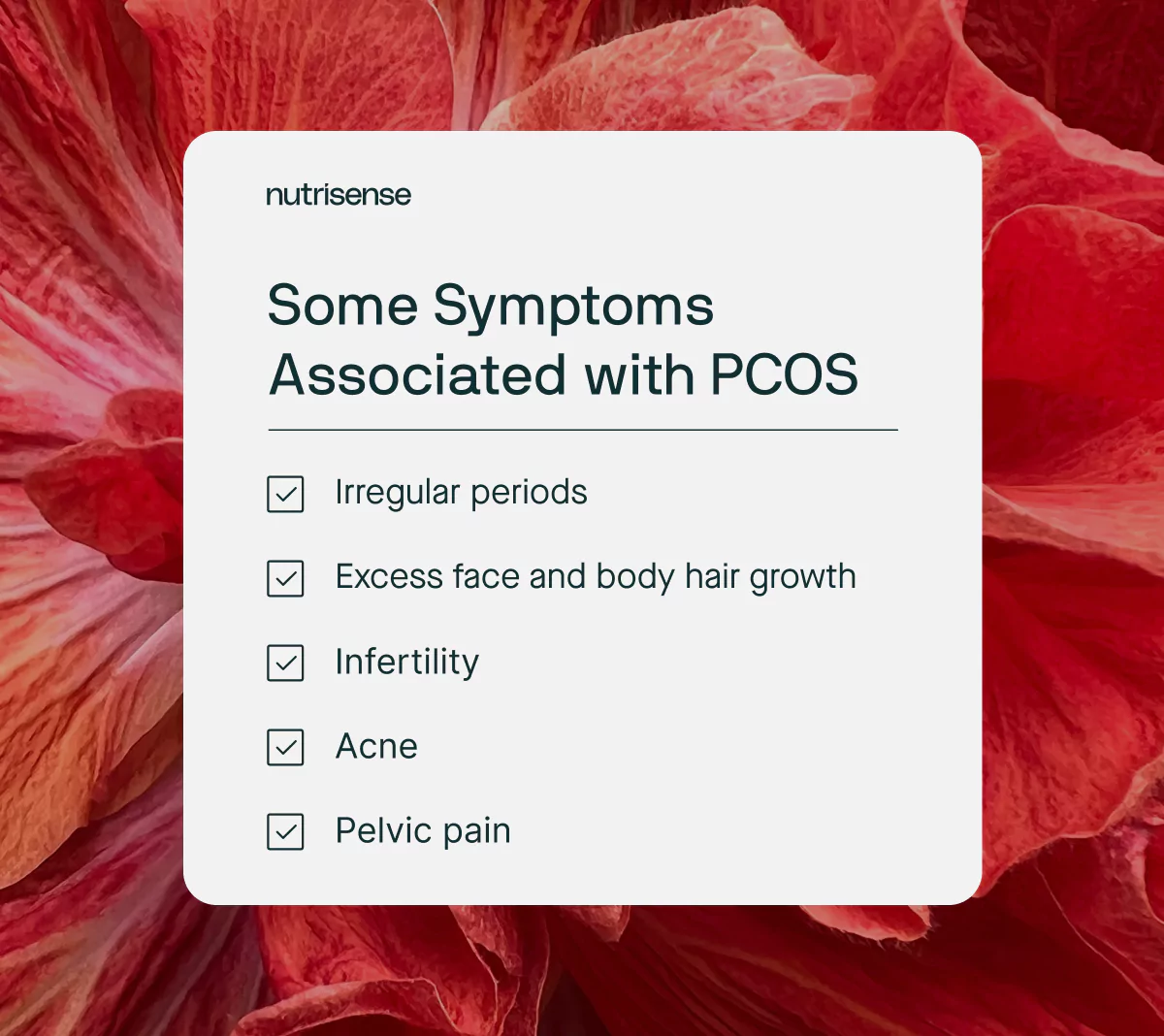
The most common symptoms of PCOS are:
- Pelvic pain
- Irregular menstrual cycles
- Excess hair growth on the face, chest, stomach, thumbs, or toes
- Baldness or thinning hair on the head
- Acne, oily skin, or dandruff
- Patches of thickened dark brown or black skin
Excess androgen levels, the lack of ovulation, and the presence of polycystic ovaries are primary diagnostic criteria for PCOS, and this condition can also cause infertility.
According to Dr. Stephanie Buck-Haskin, MD, F.A.C.O.G, OB-GYN, "PCOS causes insulin resistance, sometimes prediabetes, and excess weight gain. You can have the best chance at a healthy pregnancy with PCOS by first optimizing pre-conceptual care, as it is very important. You also should be mindful of your weight, glucose intake, and remember that exercise is very important."
Irregular Periods
Irregular menstrual cycles mean that periods may be heavier or lighter than usual, longer than 35 days or shorter than 21 days, or a lack of a period altogether. Irregular periods may be caused by many things, but with PCOS, this is often caused by disrupted ovulation and increased androgen levels, which can cause other side effects as well.
Excess Androgen Levels
Sometimes called male hormones, androgens are a group of sex hormones that have specific functions in the body. High levels of these hormones can cause excess facial or body hair or acne and affect your menstrual cycle.
Polycystic Ovaries
Ironically, polycystic ovaries are not covered in cysts as the name might suggest, but rather fluid-filled sacs known as follicles. These follicles, though harmless, remain attached to the ovaries in women with polycystic ovarian syndrome and can cause other symptoms to occur.
How is PCOS Diagnosed?

There is no single test used to diagnose PCOS. If you begin to have symptoms such as irregular periods, weight gain, or excess body hair, your healthcare provider may order blood work to check for abnormal hormone levels and perform an ultrasound to assess your ovaries. A diagnosis of PCOS can be made if you have two or more of the primary symptoms of this condition.
However, around half of women with polycystic ovaries don’t have any symptoms at all. In fact, the cysts that PCOS came to be known for are just an incidental finding when a healthcare practitioner images the ovaries - they aren’t known to cause any symptoms on their own.
A1C, Fasting Insulin, and the OGTT: What Your Lab Results Can Tell You
If you have PCOS, adding A1C, fasting insulin, and an oral glucose tolerance test can give a clearer picture of your glucose status and insulin resistance. Diagnostic thresholds for A1C, fasting plasma glucose, and the 2-hour OGTT are summarized in the ADA Standards of Care in Diabetes.
- A1C estimates average glucose over 2 to 3 months. Prediabetes is 5.7 percent to 6.4 percent. Diabetes is 6.5 percent or higher.
- Fasting plasma glucose reflects baseline morning levels. Prediabetes is 100 to 125 mg/dL. Diabetes is 126 mg/dL or higher.
- 2-hour OGTT measures the response after a 75-gram drink. Prediabetes is 140 to 199 mg/dL at 2 hours. Diabetes is 200 mg/dL or higher.
- Fasting insulin does not have a single universal target. Your clinician may use lab reference ranges or combine fasting insulin with fasting glucose to estimate insulin resistance.
If you use a continuous monitor, remember it reports glucose measured in interstitial fluid and can complement lab testing by showing day-to-day patterns between visits. Learn more in What is a CGM?
Does PCOS Cause High Glucose Levels?
According to the Centers for Disease Control, more than half of women with PCOS develop type 2 diabetes mellitus by age 40. At the same time, people with insulin resistance, type 2 diabetes, and gestational diabetes are also more likely to develop PCOS, according to research.
So why do PCOS and type 2 diabetes appear to be so connected? Studies show that PCOS patients are often insulin resistant - meaning their body is not able to use insulin effectively. With insulin resistance, your body is not able to properly respond to glucose in the bloodstream, leading to elevated glucose levels.
Risk Factors
Other risk factors for PCOS can include obesity, family history, and chronic inflammation, which are also often linked to elevated glucose levels. To find out if you have high glucose levels or insulin resistance, your doctor may order a blood test to look at your fasting glucose and fasting insulin levels.
PCOS and Prediabetes
Just as we’ve discussed above, PCOS and prediabetes are often interconnected. It may be easy to think of this connection as a sort of “chicken or the egg” dilemma, since each condition can increase the risk of the other.
People who develop PCOS may, as a result, be more at risk for developing prediabetes, and in the same way, women diagnosed with prediabetes can then have a higher risk for developing PCOS. This is why it’s so important to check in with your doctor regularly, especially if you have a family history of either condition.
If left untreated, prediabetes can develop into type 2 diabetes over time. Learn more about the warning signs of prediabetes here.
Endocrine Changes Associated with PCOS
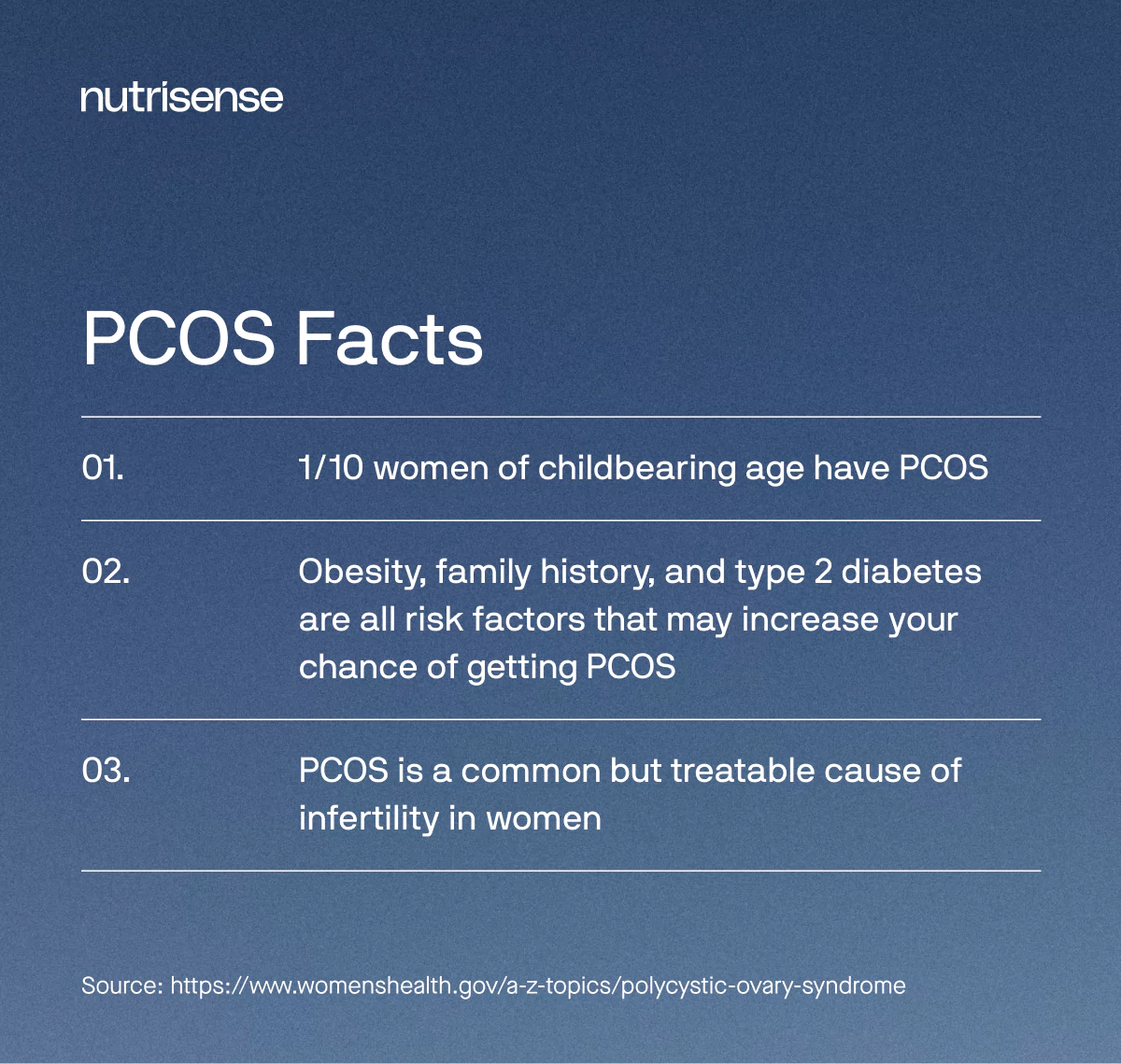
Although it only becomes symptomatic in half of the women who have it, PCOS is still the single most common cause of infertility in women. High testosterone levels can also cause excessive hair growth, known as hirsutism, usually on the face, chest, or back.
Likewise, high testosterone can cause male pattern baldness, or thinning hair and hair loss from the head, typically along a receding hairline. High testosterone levels can also cause oily skin or acne.
Beyond sex hormones, however, there are other hormone changes associated with PCOS. Although endocrinology researchers are still unsure of the exact connection, PCOS is associated with insulin resistance.
As we mentioned earlier, if your body begins to lose its insulin sensitivity, it becomes harder for you to use the glucose in your blood for energy, which can lead to chronically elevated glucose and insulin levels over time.
Conversely, if glucose levels stay chronically elevated, this can damage multiple organ systems and require more intensive medical care in later life. PCOS is also associated with high cholesterol levels, which pair exceptionally poorly with the vascular changes secondary to long-term insulin resistance.
Is There a Cure for PCOS?

Although there is no official cure for PCOS, there are dietary and lifestyle changes, as well as drug treatments, that are often recommended by doctors to make the symptoms more manageable. For some people, this can bring significant relief. Getting proper treatment is important, since PCOS can also lead to a higher risk of developing cardiovascular disease, hypertension, and metabolic syndrome.
Medication Options
Clinicians may prescribe anti-androgen therapy to help with symptoms, like body hair and acne, while fertility treatment is often successful. There are also some surgical options if medical treatment is ineffective, but these are rarely used since treatment is usually symptomatic.
Weight and BMI
Many people with PCOS, and its accompanying insulin resistance, are also either overweight or obese. Obesity or being at a higher body weight can also increase the amount of insulin your body produces, as more cells demand energy transport from the blood. Taking steps to lose weight and setting a weight loss goal may also be helpful for some people.
Lean Type PCOS
However, a “lean type” PCOS does exist and may impact some women with normal BMI. Some researchers have found that insulin resistance is inherent in PCOS regardless of BMI.
3 Tips for Supporting Healthy Glucose with PCOS
Here are Nutrisense dietitian Heather Davis, MS, RDN, LDN’s top three tips to support healthy glucose if you have PCOS.
1) Follow a Healthy Diet
Healthy foods, such as whole vegetables, complex carbohydrates, lean protein, and healthy fats, can form the backbone of a nutritious and fulfilling diet. For more dietary tips for PCOS, see our article on what to eat with PCOS here.
Consulting a registered dietitian or nutritionist can also be beneficial, as they can help you optimize your diet based on your unique health needs and create a sustainable plan that you can stick to.
2) Implement Healthy Lifestyle Changes
In addition to nutrition, regular and either low or moderate-intensity aerobic exercise can support healthy glucose regulation. Health professionals at the CDC suggest getting at least 150 minutes of exercise per week for optimal health. Get exercise inspiration for PCOS in our helpful guide right here.
While getting enough sleep and reducing stress levels can seem minuscule, these two lifestyle changes can each have a major impact on your glucose. Read more about healthy lifestyle strategies for PCOS here.
3) Consider Monitoring Your Glucose
Knowing how your glucose levels respond to your daily habits and diet can be a valuable way to manage your energy balance and support long-term health. Continuous glucose monitors (CGMs) can help automate the process of monitoring glucose levels and give you a long-term picture of your health trends.
CGMs can also show you how specific foods affect you so you can create a healthy lifestyle plan with your needs in mind. Everyone’s glucose curve is unique - that’s why it’s important to experiment and find out what works best for you.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. With Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
Expert Support for Your Plan
Sign up to access insurance-covered video calls with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Your Data, All in One Place
With the Nutrisense Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitors (CGMs), and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Take the First Step Today
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Heather is a Registered and Licensed Dietitian Nutritionist (RDN, LDN), subject matter expert, and technical writer, with a master's degree in nutrition science from Bastyr University. She has a specialty in neuroendocrinology and has been working in the field of nutrition—including nutrition research, education, medical writing, and clinical integrative and functional nutrition—for over 15 years.




