PCOS Nutrition: Food and Diet Strategies for Polycystic Ovary Syndrome

Key Takeaways
Polycystic ovary syndrome is an endocrine condition caused by hormonal imbalances—or more specifically, an increased level of androgens in the body. With this condition can come some unwanted effects, as symptoms of PCOS often include things like excess hair growth, irregular periods, and weight gain.
Proper nutrition can play a critical role in improving symptoms of many types of health conditions. In other articles, we’ve highlighted tips for what to eat with PCOS and even had a look at some non-dietary self-care techniques for PCOS that can be deployed to combat this condition.
But have you ever wondered if any of the fad diets can actually be beneficial for PCOS? And what about things like caffeine or alcohol—could they be impacting you negatively if you have this condition?
Let’s look at the different types of PCOS nutrition strategies that are often touted as ideal and what information you should actually take into consideration for your health.
What Nutrition Plan is Best for PCOS?

You’ve probably seen countless articles promoting a so-called “best diet” for PCOS nutrition. But is there really an ideal PCOS diet?
Like most people, if you have PCOS, you’ll want to pay close attention to eating whole foods, minimizing added sugar, and eating the appropriate amount of calories in a day based on your individual needs. People with PCOS should also be vigilant about limiting or avoiding refined carbohydrates, ultra-processed foods, and trans fats.
Let’s have a look at some of the dietary strategies commonly promoted as beneficial for PCOS and whether or not there’s any scientific research to back them up.
Following a Low Carbohydrate or Ketogenic Diet

For some women with PCOS, following a keto diet (or a low carb diet) may be beneficial for improving symptoms of PCOS. This may be because the keto diet has been shown to help regulate blood sugar levels and improve insulin resistance for some people.
The keto diet seeks to largely replace carbohydrates with protein and fats that can be metabolized into ketones, which many but not all organs can use as fuel instead of glucose. The amount and type of carbohydrates you are able to tolerate will depend upon your level of insulin resistance and carbohydrate tolerance.
PCOS is often linked to insulin resistance, a condition where your body has reduced insulin sensitivity and doesn’t process glucose from your blood as efficiently. However, if you have PCOS and don’t have any signs of insulin resistance, a low carbohydrate diet may not be necessary for you. Working with a healthcare provider, dietitian, or nutritionist is recommended to determine the proper diet to manage PCOS symptoms.
Regardless of whether or not someone with PCOS chooses to adhere to a low-carb diet, making a move to reduce added sugar can be one of the single most impactful changes. Higher amounts of added sugar not only increase risk for diabetes, heart disease, and obesity, but can directly impact regulation of multiple hormones.
Eating Gluten-Free and Dairy-Free Diet
Many people with PCOS turn to elimination diets such as a gluten-free or dairy-free diet. But is there any benefit to removing gluten or dairy from your diet?
There is no known link between PCOS and Celiac disease, however some women with PCOS report feeling better after removing gluten from their diet. While this is not backed up by any scientific research, individual food intolerance or sensitivities may exist.
Similarly, there is no hard link between PCOS and lactose intolerance or dairy protein allergy. However, some women with PCOS also have problems with acne and research shows that elimination of dairy can help with this for some individuals.
If you do have intolerances to gluten, dairy, or any other food, feelings of bloating, fatigue, cognitive or skin symptoms may be present and may worsen the similar constellation of symptoms associated with PCOS. Since food sensitivity tests are not very reliable, working with a professional dietitian or nutritionist with experience in assessing food sensitivities may be very helpful.
Eating a High-Protein Diet
High-protein diets have also risen in popularity in recent years, and not just among people with PCOS. Eating plenty of lean protein sources can be a valuable addition to any healthy diet, but it can be especially beneficial for women’s health.
Protein can help facilitate muscle growth when paired with physical activity or a weight lifting routine, which can help boost your metabolic rate and help you maintain a healthy weight.
At the same time, some protein sources such as fatty fish are also good sources of healthy fats known as omega 3 fatty acids, which can help reduce the risk of cardiovascular disease in people with PCOS. Protein-rich foods are also some of the richest sources of vitamins and minerals, including zinc, selenium, B vitamins, iron, and calcium.
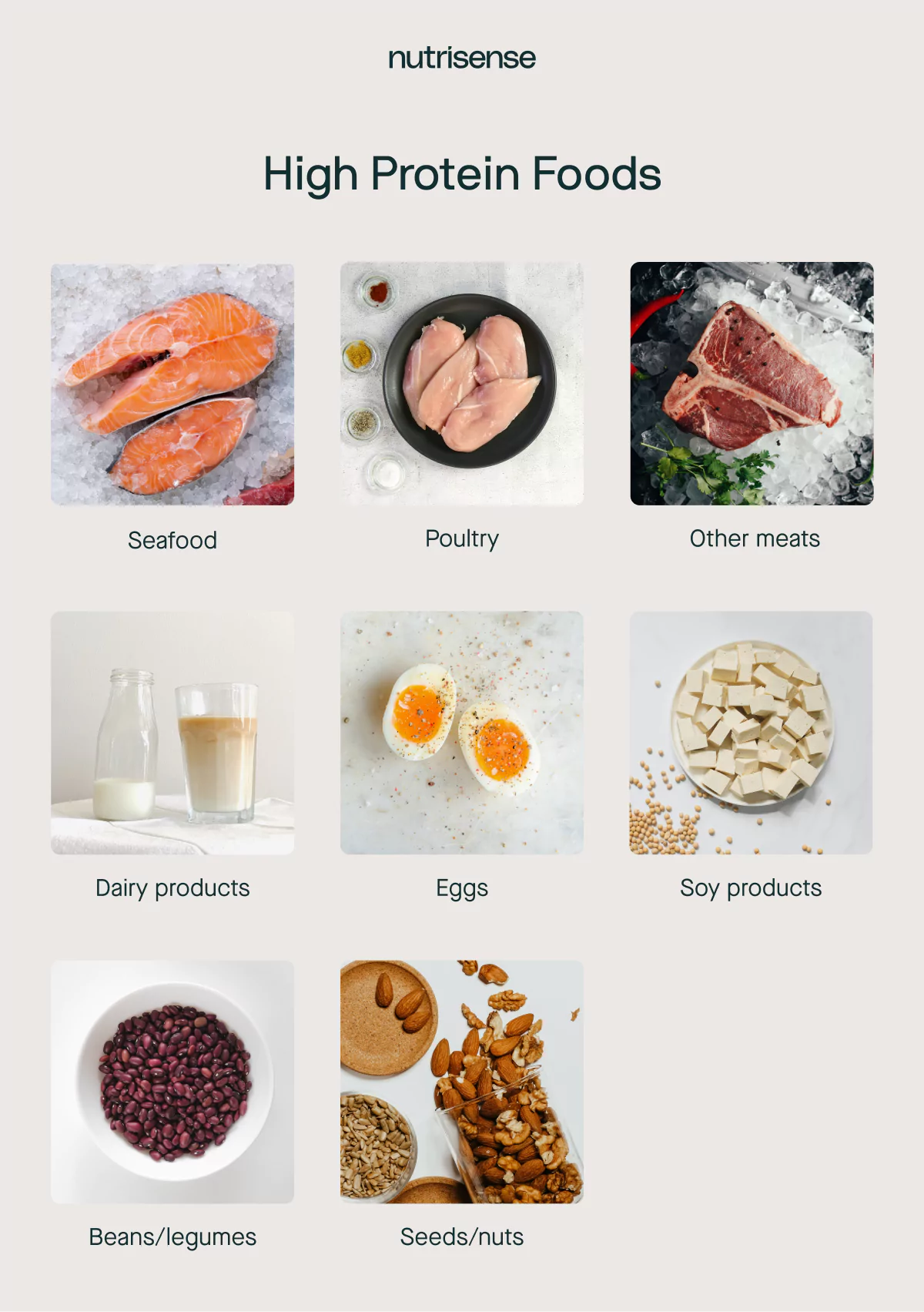
High protein foods include chicken or turkey breast, fish like salmon or sardines, eggs, tofu or tempeh, legumes such as lentils, red meat, and beans.
Following the Intuitive Eating Approach
Some people can get so focused on how to diet, what exactly to eat, and when to eat it. If the stress associated with strict adherence to a nutritional regime presents more problems than solutions, it may be time to rethink this approach.
Rather than having a list of foods to include or avoid, an intuitive eating approach encourage deepening your relationship with:
- Your hunger and fullness cues
- How your body feels before, during, and after meals
- Emotional connections, triggers, or responses to foods
Additional Nutrition Advice for PCOS

Here are a few other nutrition tips that may be beneficial for anyone suffering from this health condition.
Consider Reducing Alcohol
As we discussed in our self-care for PCOS article, making lifestyle changes such as reducing alcohol consumption can also be beneficial for this condition. One of the central problems associated with PCOS is that cortisol levels are often persistently elevated and estrogen metabolism may be dysregulated.
Alcohol may negatively impact both of these aspects, as well as other metabolic functions. Stress is often “self-medicated” with alcohol, which can be particularly harmful in the case of PCOS.
Consider Reducing Caffeine

The combination of sluggishness and high stress can be challenging to navigate with caffeine. On the one hand, caffeine can boost energy levels in the short to medium term. However, caffeine doesn’t actually supply the building blocks for energy production in your body and simply pushes the body to work harder with the resources it already has.
For some people, caffeine may also encourage increased cortisol levels and may impact estrogen metabolism.
Address Intolerances and Allergies
Although mentioned earlier, it’s worth emphasizing that specific foods can have an influence on energy levels, inflammation, and stress. If someone with PCOS has a known allergy or intolerance, reducing or eliminating this trigger is one impactful change they can make in their diet.
PCOS and Insulin Resistance

According to the Centers for Disease Control, many people with PCOS also have insulin resistance, which means their body struggles to properly process sugar. The result is that blood glucose levels become elevated above normal levels, with two significant consequences.
Persistently high blood glucose levels can have a negative impact on a variety of different areas of your health. These changes can lead to other conditions, such as type 2 diabetes, obesity, high blood pressure, and even heart disease.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Kara Collier is a registered dietitian nutritionist and certified nutrition support clinician who is passionate about reshaping how we approach prevention, behavior change, and metabolic health. A Forbes 30 Under 30 honoree, she’s helped over 150,000 people improve their metabolic health using tools like continuous glucose monitors and behavior-focused nutrition strategies. Kara has been featured by Forbes, UC Berkeley, and HLTH, and has appeared on top podcasts like Mind Pump and The Genius Life.




