How to Lower A1C Levels Naturally: 8 Proven Ways

Key Takeaways
- Prioritize Protein & Fiber: Eating nutrient-dense meals prevents rapid glucose spikes.
- Exercise Consistently: Aim for 150 minutes of weekly activity to improve insulin sensitivity.
- Manage Stress: Chronic stress releases cortisol, which can raise glucose baselines.
- Sleep Well: Quality sleep is essential for metabolic recovery.
- Monitor Glucose Variability: Using a CGM helps you spot and reduce daily spike.
- Prioritize Protein & Fiber: Eating nutrient-dense meals prevents rapid glucose spikes.
- Exercise Consistently: Aim for 150 minutes of weekly activity to improve insulin sensitivity.
- Manage Stress: Chronic stress releases cortisol, which can raise glucose baselines.
- Sleep Well: Quality sleep is essential for metabolic recovery.
- Monitor Glucose Variability: Using a CGM helps you spot and reduce daily spike.
Why monitor A1C without diabetes?
Getting your A1C levels tested regularly is important if you are at risk of prediabetes or type 2 diabetes. But what if your A1C levels are high and you don’t have diabetes?
There are a few reasons why you may have high A1C levels that aren’t related to diabetes. There may even be some reasons why A1C readings may be inaccurate. For this reason, it may be important to assess and explore more than just your A1C level when determining your risk for things like prediabetes and diabetes.
Before these markers progress to other health problems, making healthy lifestyle interventions can support lower A1C levels and consequently reduce your risk of diabetes developing down the line.
Wondering what strategies you can use that might help you keep your A1C levels in a healthy range? Read on to learn more about healthy A1C levels and what you can do to improve your overall health and wellness.
What are A1C Levels and Why Do They Matter?
Your A1C level, also called hemoglobin A1C or HbA1C, is a measurement of your average glucose level over the past 3 months. Instead of measuring the amount of glucose in your bloodstream, your A1C level represents the percentage of hemoglobin in your red blood cells that is coated in sugar.
Hemoglobin is a protein found in your red blood cells. When glucose enters your bloodstream, it can attach itself to hemoglobin. Everyone has some amount of sugar attached to the hemoglobin in their blood cells, but people with high glucose levels have more.
Health risks
If your A1C results are on the rise, you could be more at risk of developing prediabetes, cardiovascular disease, kidney disease, and other metabolic conditions.
Hyperglycemia symptoms to watch for
Changes in glucose can show up as everyday signs. If you notice the symptoms below consistently, check in with your clinician for testing and next steps.
- Persistent thirst and frequent urination, including overnight trips
- Headaches or blurred vision
- Fatigue after eating, energy dips, or restlessness
- Tingling or numbness in hands or feet
- Slow-healing cuts or sores, gum irritation, or more frequent infections
- Unexplained weight loss or increased hunger
- Dry mouth or skin changes
A1C ranges
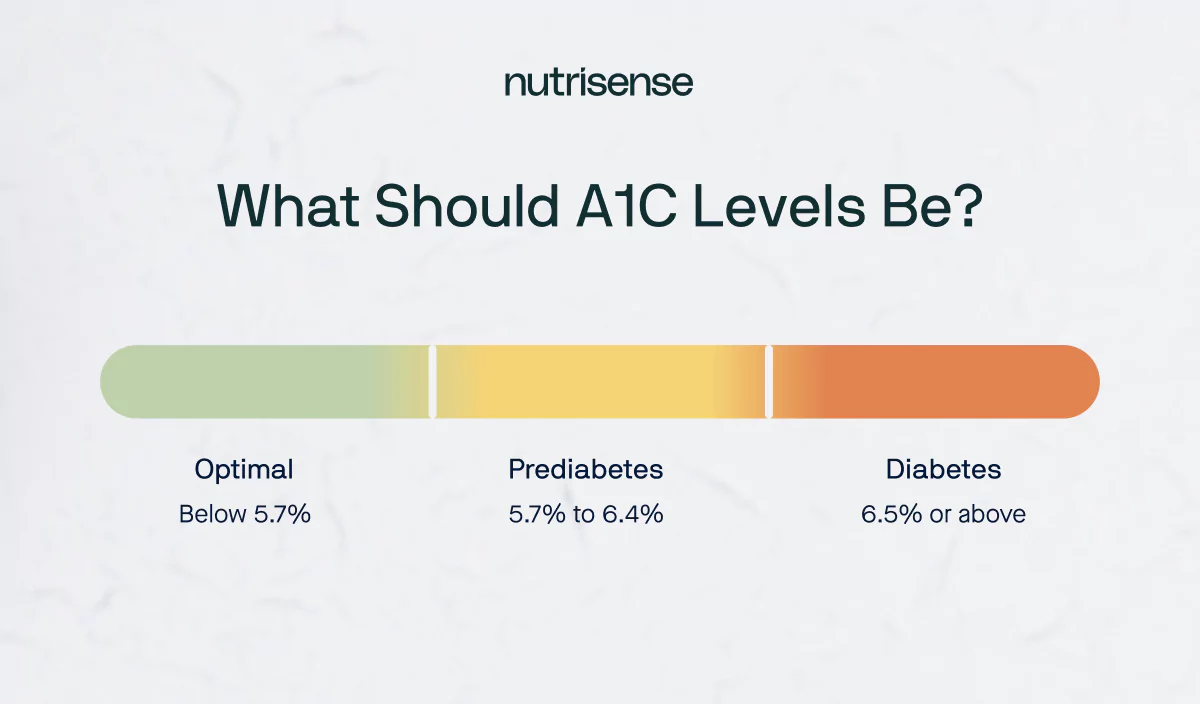
A blood test of your A1C levels (or average glucose level) is used to diagnose prediabetes and diabetes. The A1C test is also used to help people with diabetes and their healthcare teams manage their condition.
According to the American Diabetes Association, these are the ranges of A1C levels:
- An A1C level of 5.7 percent or below is considered normal
- An A1C level between 5.7 and 6.4 percent is considered prediabetes
- An A1C level of 6.5 percent or higher is considered diabetes
Goals and testing
If you have a higher-than-normal A1C level, you should work with your healthcare provider to determine an A1C goal based on your unique needs. If you’ve not gotten your A1C levels tested recently, check out our handy calculator to see how you can calculate an estimate of your A1C value.
Why is my A1C high without diabetes?
If you don’t have diabetes, there are a few reasons why your A1C levels could be high. Some other medical conditions can affect A1C levels or cause falsely high readings during an A1C test.
Anemia and Other Deficiencies
Iron deficiency anemia is a common condition that is associated with falsely elevated A1C levels. Studies have also shown that anemia that occurs as a result of vitamin B12 and folate deficiencies can also raise A1C levels. Asplenia, or disorders of the spleen, also raise A1C levels.
Certain Health Conditions
Hypertriglyceridemia (too many fats in the blood), hyperbilirubinemia (also called jaundice), and uremia (abnormally high levels of waste in the blood, caused by kidney dysfunction) can all falsely elevate A1C levels.
Medications that affect A1C
Finally, some medications and chemicals can falsely elevate A1C. This can include lead poisoning, salicylates like aspirin, opioids, and ingestion of vitamin C.
That "Slightly High" Lab Result
Your latest lab report is back, and your A1C is 5.8%. It’s frustrating because you’ve been trying so hard to eat well and stay active. This single number reflects your average glucose over the last three months, showing that your daily efforts might not be adding up the way you thought.
This result is not a final verdict, but a starting point for understanding how your body responds and what small, consistent changes can make a difference. As one member shares: “I feel better, I’m sleeping better, I have more energy”.
8 Ways to Lower A1C Levels Naturally
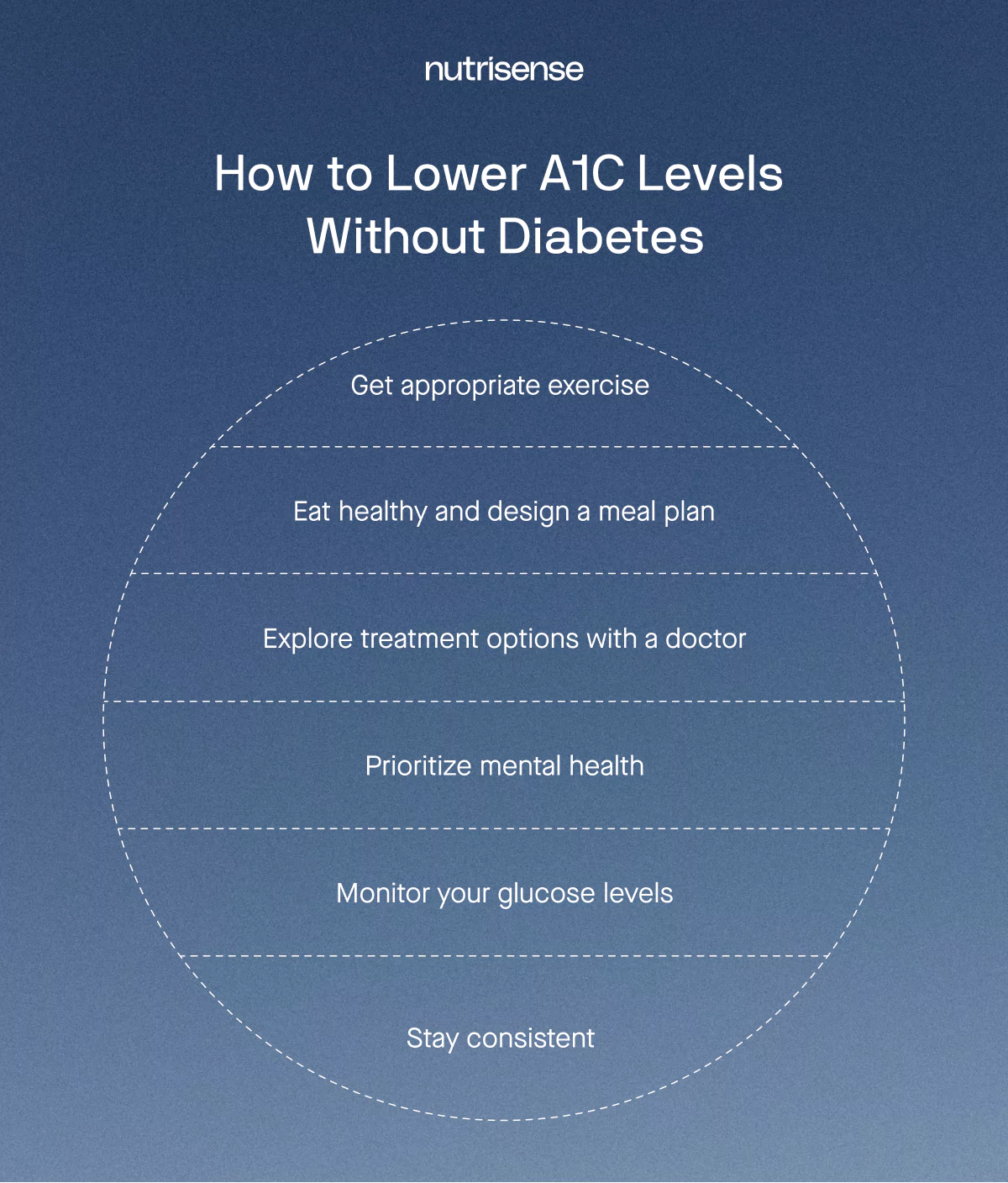
If you don’t have diabetes but your levels are high, focusing on glucose variability is key. Here are 8 evidence-based ways to lower your A1C:
1) Eat balanced meals
Eating a healthy diet is one of the most important things you can do when it comes to managing glucose. This can include a focus on protein, non-starchy vegetables, whole grains, and low-fat dairy or fortified dairy alternatives, while limiting refined carbs and sugary foods and drinks.
Because your body breaks down most carbohydrates into glucose, the amount and type of carbs you eat have a high impact on your glucose. Certain carbohydrates, including added sugars, white rice, and bread products that contain white flour, are absorbed by the body very quickly and can lead to higher and/or more frequent spikes in glucose if eaten consistently.
Fiber and protein

When it comes to maintaining healthy glucose levels, fiber and protein can both play a crucial role. Fiber is a carbohydrate that isn’t digested or absorbed by the body, and it can help keep you satiated and slow down the absorption of glucose in your blood.
Fiber is mainly found in nutrient-rich plant foods, like:
- Fruits and vegetables
- Legumes
- Whole grains
Protein is also a crucial part of a healthy diet. It is required by the body to help build and repair tissue, make and regulate hormones, and maintain organ function. Protein can also help keep glucose levels stable. Here are some good sources of lean protein to consider including in your diet:
- Beans and lentils
- Fish and seafood
- Eggs
- Uncured and lean red meats and poultry
2) Plan your meals

Designing a meal plan with a dietitian or nutritionist can be a great way to make sure you are getting enough nutrient-dense foods in your diet. A meal plan can also help you recognize the amount of food you are actually eating and monitor your portion sizes.
When it comes to meal planning, the USDA recommends:
- Write down the meals you plan to have and when, including breakfast, lunch, dinner, and snacks.
- Take note of what you already have in your freezer, pantry, and fridge.
- Make a grocery list such as this prediabetes food list, and organize it by food group to make shopping easy.
- Buy a combination of fresh, frozen, and non-perishable foods. Eat the fresh foods first so they don’t go bad, and stock your freezer and pantry with items you can eat later.
- Plan for leftovers by making larger recipes so you’ll have enough servings for more than one meal.
3) Personalize your fitness
A lack of appropriate exercise can lead to an increased risk of high glucose. When you exercise, your cells’ sensitivity to insulin increases to better enable your body to use the available glucose in your blood.
Even if you have no available insulin, your cells are able to use glucose for energy when your muscles contract during physical exercise. Moderate activity, like walking, stretching, and moderate weight lifting with light weights, is the most likely to positively affect glucose.
But more exercise isn’t always better for glucose balance. If you are overtraining or improperly fueling for workouts, this added stress can potentially impair glucose tolerance. It’s all about finding the right approach for your body.
4) Work with an expert
It’s always important to consult a doctor and a qualified nutritionist when it comes to making decisions about your health and diet. Only a qualified health professional can diagnose and treat serious health conditions.
As a member at Nutrisense, you are paired with a complimentary nutritionist to help you set sustainable goals and stay accountable to them. They can also offer you expert advice on how to design and stick to a healthy diet or exercise routine to support balanced glucose and benefit your overall health.
5) Medications and supplements
If you’re having trouble lowering your glucose with dietary changes or lifestyle interventions, your doctor may prescribe medications to help. There are several medications that are often used to treat high A1C or glucose levels. These include things like alpha-glucosidase inhibitors, biguanides, bile acid sequestrants, dopamine-2 agonists, DPP-4 inhibitors, and more.
Though some supplements like berberine have been used to lower glucose levels, it’s wise to consult a qualified healthcare provider before beginning any supplements. Some supplements, like melatonin or others, may have the potential to raise glucose levels in certain people. It’s also worth considering that any drug or medication that is poorly tolerated by the body may trigger a stress response, which may contribute to elevated glucose for some people.
6) Prioritize mental health

Stress of many kinds can be a major factor in managing glucose levels. It can cause your body to release cortisol, which in turn often elevates glucose.
Chronic stress can lead to insulin resistance, which makes it harder for your cells to use glucose as energy. To learn more about some of the symptoms of chronic stress and learn some tips for managing it, take a look at our article on managing stress.
7) Monitor your glucose

Checking your glucose often is a good way to make sure you are informed about your glucose levels and prevent glucose spikes. A continuous glucose monitor, or CGM, is a tool that can give you glucose readings throughout the day.
A CGM is a small sensor that stays on the back of your arm and measures your glucose levels 24/7. Knowing how your glucose reacts to certain lifestyle factors like diet and exercise can be a powerful tool in maintaining healthy lifelong habits.
8) Be consistent
Remember that your A1C levels are a reflection of your glucose over time. Making consistent healthy choices is the best way to form habits that keep your glucose at healthy levels. It can also take a while to see results, so don’t give up if you don’t see changes right away. Keep going and don’t get discouraged!
How long does it take to lower A1C?
It typically takes 3 months. Because A1C measures glucose attached to red blood cells (which live for about 3-4 months), you won't see changes overnight. However, you can lower your average daily glucose immediately, which will eventually result in a lower A1C.
Find the right Nutrisense programto turn insight into progress.
Frequently Asked Questions
What foods lower A1C quickly?
No single food lowers A1C instantly, but high-fiber foods like leafy greens, legumes, and chia seeds slow glucose absorption. Pairing carbohydrates with protein can also blunt spikes.
Does drinking water lower A1C?
Staying hydrated helps your kidneys flush out excess glucose through urine. While it doesn't "cure" high A1C, dehydration can cause glucose levels to concentrate and rise.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. With Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
1:1 guidance that fits your day
Sign up to access insurance-covered video calls with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitors (CGM), and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Start your quiz
Ready to take the first step? Take our quiz to find the right Nutrisense program to help you take control.

Heather is a Registered and Licensed Dietitian Nutritionist (RDN, LDN), subject matter expert, and technical writer, with a master's degree in nutrition science from Bastyr University. She has a specialty in neuroendocrinology and has been working in the field of nutrition—including nutrition research, education, medical writing, and clinical integrative and functional nutrition—for over 15 years.


.webp)

