The Best Diet for Non-Diabetic Hypoglycemia

Key Takeways
A lot can happen to your body when your glucose levels are unbalanced. One of the conditions you can develop when they're too low is hypoglycemia.
Although this condition is usually associated with having type 1 and type 2 diabetes, it can also happen to people without diabetes. If you have symptoms of this condition, it's a good idea to consult with a healthcare professional and learn to manage your blood sugar level with the help of a glucose monitor.
Because everyone may exhibit different symptoms, it can be tricky to diagnose without the help of an invasive finger-prick test. Luckily, you can also track your blood glucose levels using a tool like a continuous glucose monitor (CGM).
You can use a CGM without diabetes to help you keep an eye on your glucose levels and make healthier lifestyle decisions for your overall well-being. So, if you're wondering about the different types of hypoglycemia, how you can change your diet to manage symptoms, and where glucose monitoring fits into all of this, read on to learn more.
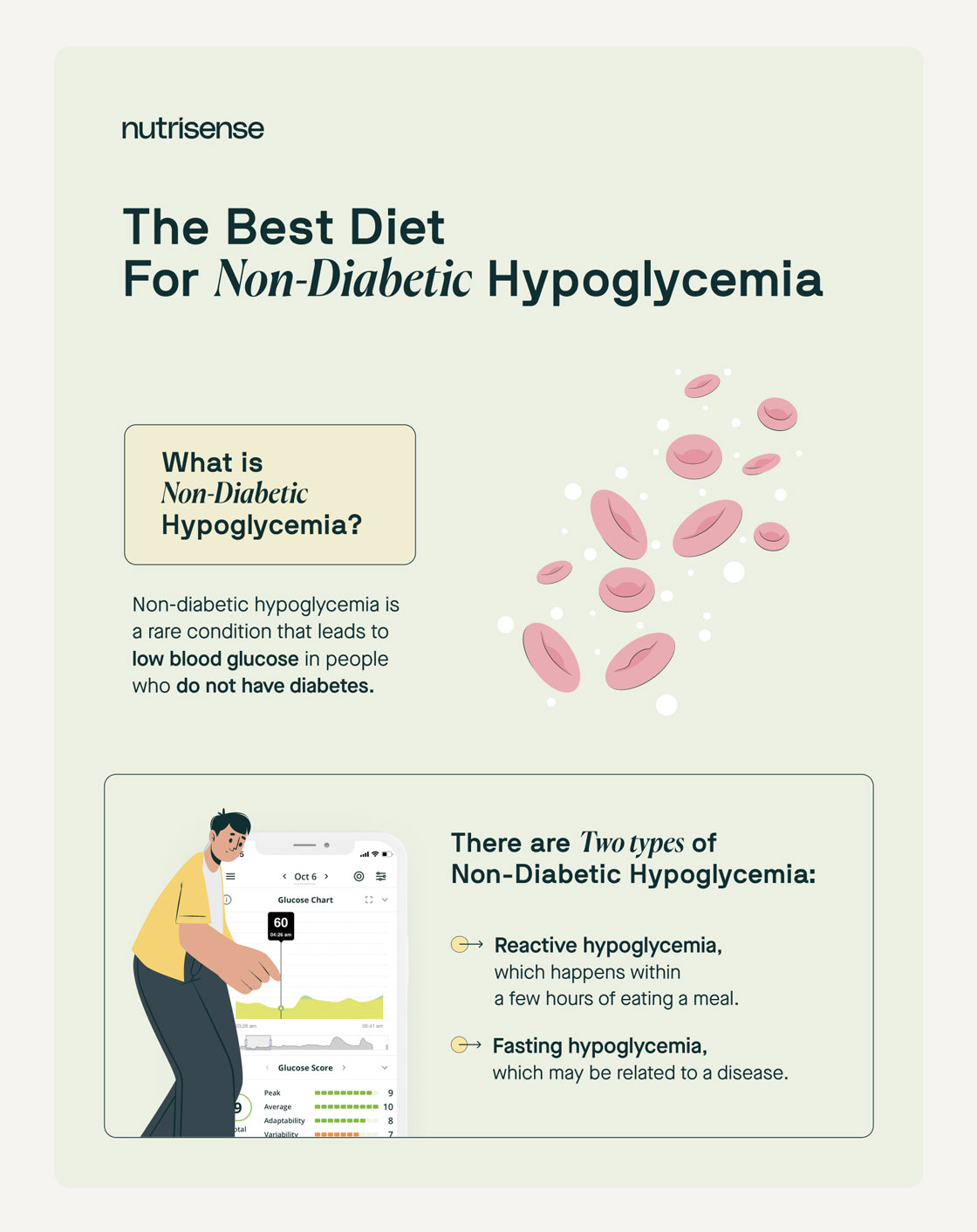
What Is Non-Diabetic Hypoglycemia?
Non-diabetic hypoglycemia occurs when blood glucose levels drop below the normal range of 55 milligrams per deciliter (mg/dL). There are two types of non-diabetic hypoglycemia that you should be aware of:
- Reactive Hypoglycemia (postprandial hypoglycemia): Blood glucose levels can sometimes drop after eating a meal. This is known as reactive hypoglycemia. It usually occurs within the first four hours following a meal. In some instances, reactive hypoglycemia can be a warning sign of prediabetes. This is especially true for people with a family history of diabetes.
Fasting Hypoglycemia (non-reactive hypoglycemia): This isn't related to meals and occurs during a fast or while you're sleeping. Some potential causes of fasting hypoglycemia include specific medications, thyroid problems, pregnancy, menopause, and other health conditions.
Signs and Symptoms of Hypoglycemia
For people with diabetes, glucose levels below 70 mg/dL are considered low. However, people without diabetes may have glucose readings of less than 70 mg/dL and still feel fine. It is only when your blood sugar drops below 55 mg/dL that your brain sends signals to your body that something is off. If you experience hypoglycemia, you may encounter the following symptoms:
- Hunger
- Crankiness
- Blurry vision
- Pale and clammy skin
- General weakness
- Numbness in arms and legs
- Cold sweat
- Lightheadedness
- Anxiety
- Brain fog
- Stuttering or slurring of words
- Headaches
- Polydipsia (extreme thirst)
- Inability to focus
- Loss of consciousness
If you experience symptoms of hypoglycemia, it's crucial to discuss them with your healthcare provider. They'll provide the necessary support and guidance to help you identify the underlying cause and explore suitable treatment options. Remember, you're not alone in this journey towards better health.
Can a Non-Diabetic Have Low Blood Sugar?
Non-diabetic hypoglycemia can affect people for several reasons. However, you are more at risk if you:
.jpeg)
- Have a family history of diabetes
- Have prediabetes
- Are obese
- Have other health problems such as anorexia, kidney disease, adrenal glands or pituitary glands issues, and pancreas problems
- Went through stomach surgery procedures, including some weight loss and bariatric surgeries like gastric bypass surgery
- Take medications such as insulin, Ozempic, antibiotics (quinine, Bactrim, gatifloxacin, pentamidine, fluoroquinolones), indomethacin, beta-blockers, anticonvulsants (gabapentin), antihistamine (hydroxyzine), cibenzoline, quinidine, bile acid sequestrants, ACE/inhibitors, and salicylates
- Drink alcohol excessively
What Is the Treatment for Non-Diabetic Hypoglycemia?
The approach to treating non-diabetic hypoglycemia varies based on several factors, including your dietary habits, past and present health conditions, and individual symptoms and body composition.
When diagnosing non-diabetic hypoglycemia, your doctor will carefully review your medical history and conduct a series of blood tests. If reactive hypoglycemia is suspected, they may suggest a mixed-meal tolerance test (MMTT), which can provide valuable insights.
Rest assured that medical treatment isn't usually required for reactive hypoglycemia. Instead, dietary or lifestyle changes are recommended to lessen the symptoms. If you have severe hypoglycemia or hypoglycemia related to diabetes, you may need medication to manage your blood glucose.
What Is the Hypoglycemic Diet?
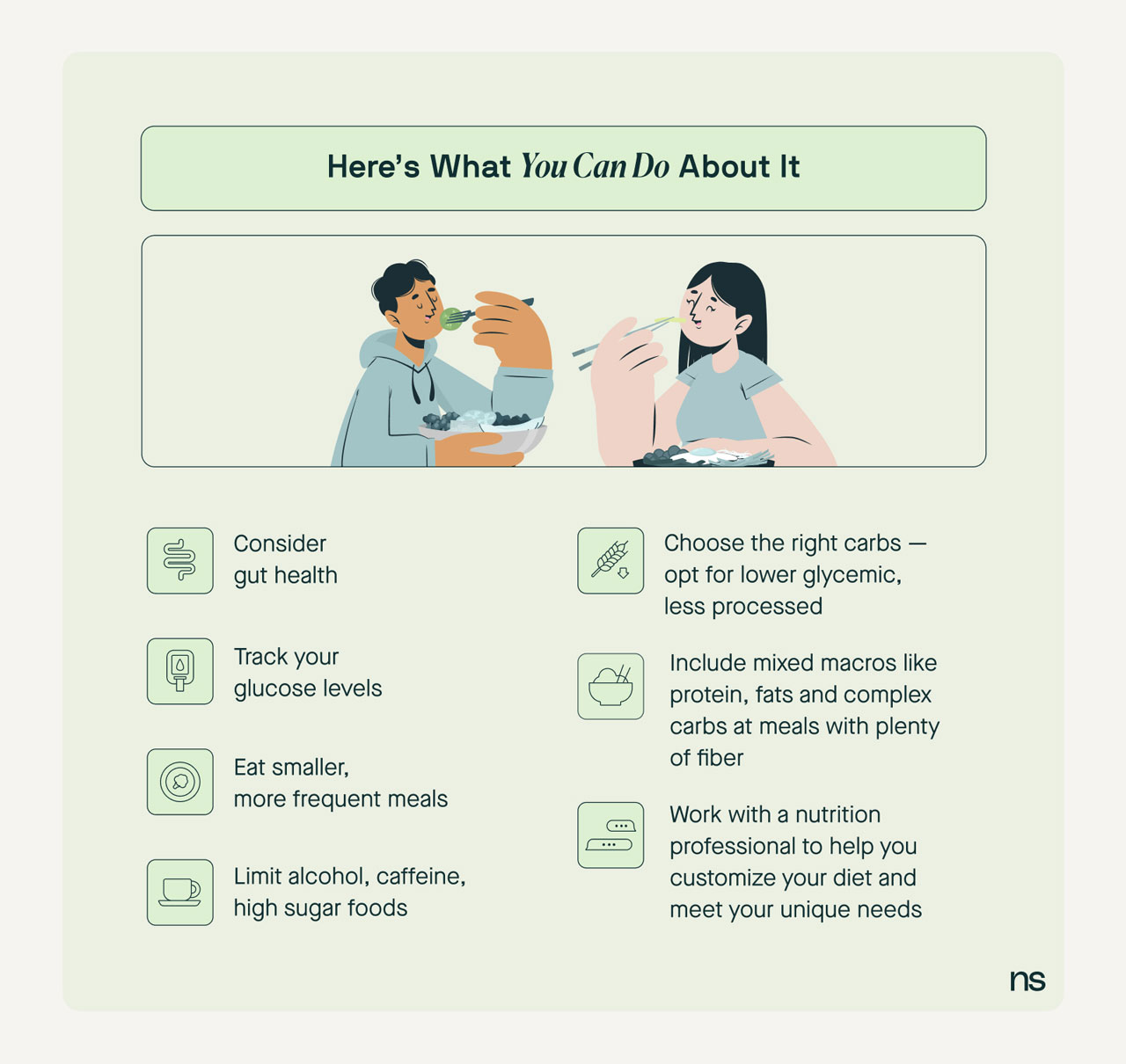
While there is no specific "hypoglycemic diet," there are some tips and tricks that may help manage your blood sugar levels. These include:
Have Small Meals and Snacks
Are you accustomed to consuming large meals three times a day? It might be worth considering a different approach. One option is to space out your meals or snacks to approximately every three hours, which can help regulate your blood glucose levels.
Remember, this approach may not be suitable for everyone. Feel free to consult your doctor or nutritionist to determine the best eating pattern for you.
Eat a Well-Balanced Daily Diet

To support your well-being and promote stable blood glucose levels, it's important to include a variety of foods including protein sources (both meat and non-meat options), dairy products (if tolerated), and lots of fiber. Consuming an appropriate amount of high-fiber foods may also help regulate blood sugar levels by slowing down digestion.
Lower Carb Intake
Recent research suggests that a lower carb, higher protein diet is helpful for people with prediabetes and type 2 diabetes, and for people with a history of gastric bypass. However, a low carb, high protein diet may not be suitable for people with hypoglycemia.
A 2022 study found that a low glycemic index diet and a Mediterranean-style diet, paired with the support of a nutritionist, led to positive results and less hypoglycemic events.
Before making any significant dietary changes, it's always best practice to consult a healthcare provider. They can closely track your condition and help you determine the best diet for your specific needs.
Minimize Alcohol Consumption
Excess drinking can cause hypoglycemic symptoms. If you drink alcohol, avoid sugary drinks, and remember to drink with food since that'll help your stomach absorb it slowly.
Limit Caffeine Intake
Caffeine can lead to a boost of adrenaline throughout the body. This boost in adrenaline may mimic hypoglycemia by increasing heart rate, sweating, and tingling. If you consume a lot of caffeine, consider reducing your intake throughout the day.
Choose the Right Carbohydrates
The glycemic index measures how much a carbohydrate raises your blood glucose levels and how quickly it does this. Including foods with a low glycemic index in your diet can help regulate blood glucose levels.
Complex carbohydrates have a lower glycemic index. Examples include:

- Whole grains like brown rice and steel cut oats
- Vegetables like broccoli, potatoes, and corn
- Legumes like beans, peas, and lentils
- Fruits like bananas and apples
Refined carbohydrates have a high glycemic index and can quickly impact glucose. Examples include:
- White bread
- Fruit juices
- Sugar-sweetened beverages like soda and sports drinks
Aim for 30–60 grams of complex carbs at each meal, and one to two 15–30 grams as a snack. By making these choices, you can effectively manage your blood sugar levels and support your overall well-being.
Of course, none of this is written in stone because everyone has a unique response to carbohydrates. If you want to take guessing out of your diet, you can easily track your blood sugar responses with the help of a CGM.
What to Eat When You Have a Hypoglycemic Episode
If you have a hypoglycemic episode, you can follow the 15:15 rule. Here's how to do it in four easy steps:
- Consume 15 grams of glucose/carbohydrates. This can be in the form of a glucose tablet, glucose gel tube, one tablespoon of sugar or honey, or a few hard candies, like a Lifesaver or Jolly Rancher.
- Wait for 15 minutes.
- Measure your blood glucose levels with a CGM.
- Repeat this treatment until your blood glucose levels reach at least 70 mg/dL.
When experiencing a hypoglycemic event, it's best to avoid high-fat foods like chocolate or cookies. They don't raise blood sugar quickly enough because the fat can delay how quickly your body absorbs the required sugar.
Remember, these are just short-term fixes for hypoglycemia. If you're looking for a way to address the root cause and prevent further blood glucose drops, consider using a CGM.
What Is the Best Food to Eat When Your Blood Sugar Is Low?
If you suffer from frequent hypoglycemia, you may want to carry a snack with you at all times. Make sure you don't go for long periods without eating. Snacks with fast-acting carbs such as hard candies, a packet of honey, or glucose gels can be helpful to carry with you.
A Hypoglycemia Food List
Choosing low glycemic index foods can help you control your blood glucose levels. Something to remember when you're planning your meals: meat and fish don't have a glycemic index because they don't have any carbohydrates.
Foods containing carbohydrates have low, moderate, and high glycemic index options. Here's a breakdown of a few of these, just to give you an idea of the best types of foods to choose from:
Bread
- Low GI: Spelt bread, sourdough bread, whole grain tortilla, heavy-mix grain bread.
- Moderate GI: Chapati, linseed bread, flaxseed bread, pita bread, pumpernickel bread, roti, rye bread, whole-grain wheat bread.
- High GI: White and whole wheat bread, naan bread.
Cereals
- Low GI: All-bran, oat-bran, steel-cut oats.
- Moderate GI: Instant, quick, or large-flake oats.
- High GI: Cornflakes, Rice Krispies, Puffed Wheat, Cream of Wheat, Special K.
Grains
- Low GI: Barley, bulgur, firm/al dente pasta, quinoa, pulse flours, mung bean noodles.
- Moderate GI: Basmati rice, brown rice, cornmeal, couscous, rice noodles, wild rice, short/long-grain white rice.
- High GI: Jasmine rice, Japanese rice, millet, sticky rice, instant white rice.
Other Starches
- Low GI: Peas, popcorn, sweet potato, winter squash.
- Moderate GI: Beets, corn, parsnip, potato, rye crackers.
- High GI: Carrots, instant mashed potato, pretzels, rice cakes, soda crackers.
Fruits
- Low GI: Apple, apricot, unripe/green banana, berries, cantaloupe, grapefruit, honeydew melon, mango, orange, peach, pear, plum, pomegranate, prunes.
- Moderate GI: Ripe banana, cherries, cranberries, figs, grapes, kiwi, lychee, pineapple, and raisins.
- High GI: Brown/overripe banana, watermelon.
Milk and Yogurt
- Low GI: Almond milk, two percent cow's milk, frozen yogurt, Greek yogurt, soy milk, and yogurt.
- Moderate GI: N/A
- High GI: Rice milk.
Beans, Peas, and Lentils
- Low GI: Baked beans, chickpeas, kidney beans, lentils, mung beans, romano beans, soybeans/edamame, split peas
- Moderate GI: Ready-made lentil or split pea soup
- High GI: N/A
Alongside low glycemic index foods, you can also consider:
- High-quality protein (meat, fish, or eggs).
- Alternative sweeteners such as stevia instead of sugar.
- Fresh vegetables, especially dark leafy greens
Does Exercise Help Reactive Hypoglycemia?
Engaging in regular exercise is always a good idea for overall health, but it can also be beneficial for managing reactive hypoglycemia. Intense or prolonged physical activity can lead to a decrease in blood glucose levels for certain individuals. If you often encounter hypoglycemia, you may need to adjust your diet based on your exercise routine.
The best way to manage this is to eat a snack containing carbohydrates and protein before exercising. Keep the snack small, and remember to stay hydrated with plenty of water throughout your physical activity. Examples of pre-exercise snacks include:
- Greek yogurt and berries
- A small amount of mixed dried fruits and nuts
- An apple and some peanut butter
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Kara Collier is a registered dietitian nutritionist and certified nutrition support clinician who is passionate about reshaping how we approach prevention, behavior change, and metabolic health. A Forbes 30 Under 30 honoree, she’s helped over 150,000 people improve their metabolic health using tools like continuous glucose monitors and behavior-focused nutrition strategies. Kara has been featured by Forbes, UC Berkeley, and HLTH, and has appeared on top podcasts like Mind Pump and The Genius Life.


.webp)

