Understanding the Effect and Function of Insulin in the Brain

Key Takeaways
Insulin is a hormone that plays an important role in regulating metabolic action throughout many areas of the body, including the brain. Insulin resistance can have dire consequences for your health, leading to an increase in the risk for conditions like:
- Obesity
- Heart disease
- Diabetes
- PCOS
- High blood pressure
But did you know that insulin resistance can negatively affect the brain as well? Read on to learn more about how insulin acts in the brain and how you can support healthy insulin levels in your body.
A Quick Overview of Insulin’s Role in the Body
In a nutshell, insulin is a hormone that helps the body move glucose from the blood into the cells. Without insulin, glucose wouldn’t be able to get into the cell to fuel energy production and other processes that keep you alive.
Insulin is produced in the pancreas, often in response to having just eaten a meal. Your body’s release of insulin depends on many things, such as the presence of carbohydrates and protein in your meal and how your pancreas is functioning.
If you have insulin resistance, your cells have a difficult time responding to the action of insulin, even if your pancreas might be making plenty of it.
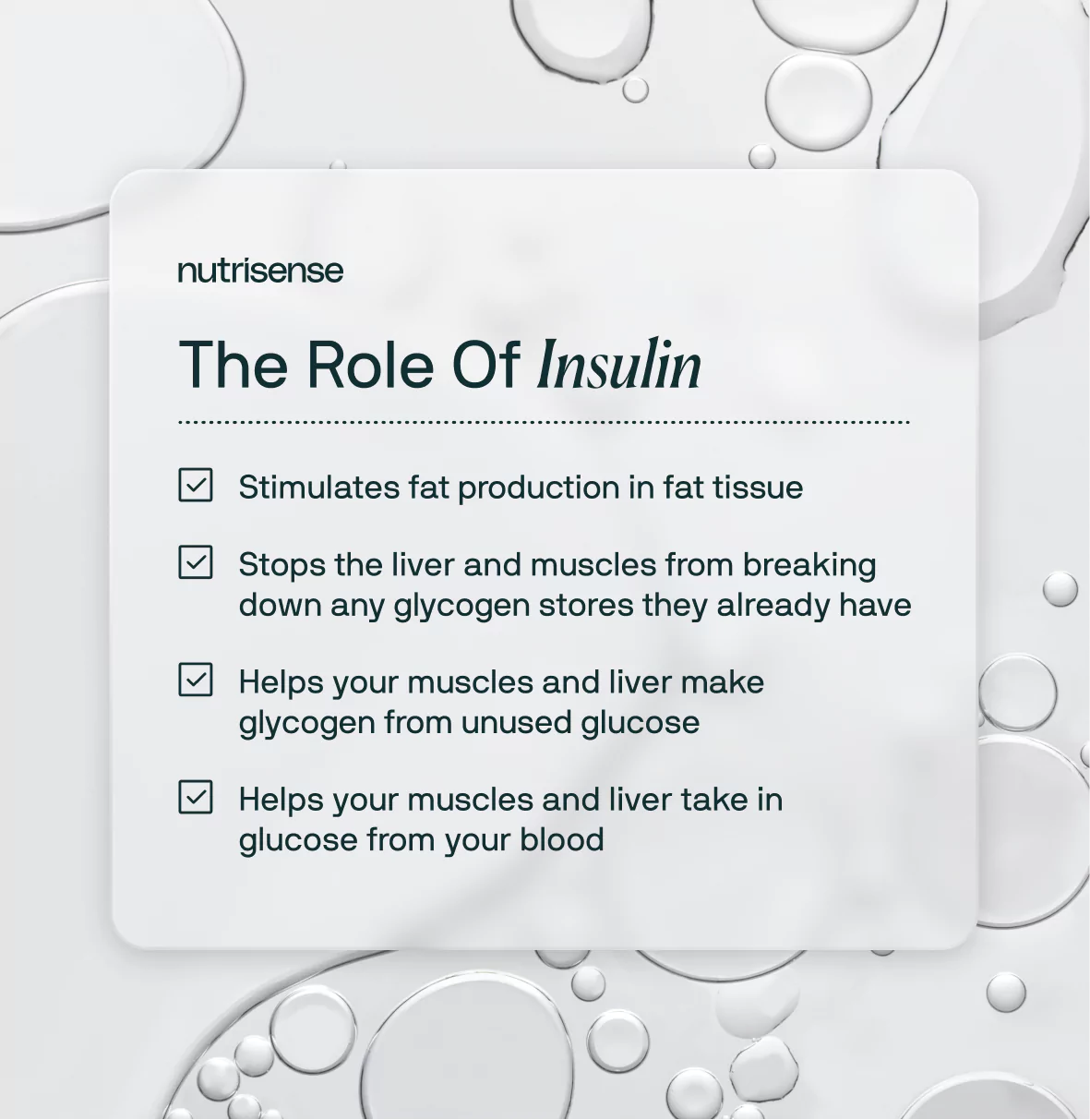
The effects of insulin in the body include:
- Helping your muscles and liver take in glucose from your blood
- Helping your muscles and liver make glycogen from unused glucose
- Stopping the liver and muscles from breaking down any glycogen stores they already have
- Stimulating fat production in fat tissue
Causes of Insulin Resistance
Insulin resistance is a complex physiological change that occurs over years and is marked by two changes. These are either an increase in insulin levels (hyperinsulinemia), or decreased insulin sensitivity in your cells
But what exactly leads to insulin resistance? Determining the exact cause of insulin resistance in each person isn’t always straightforward. Some common causes include:
- Family history or genetics
- General excess weight or body fat, especially visceral fat
- Poor diet
- Inactivity
- High stress
- Certain medications
While insulin resistance can increase your risk for being overweight or obese, not everyone with insulin resistance will be overweight or obese.
How Does Insulin Enter the Brain?
Once upon a time, many people thought that the brain was an insulin-independent organ. However, new research has shown that this is far from the case and the brain can be heavily influenced by insulin.
Does insulin in the brain come from the brain or central nervous system itself? This is a question still under investigation.
However, several studies have confirmed that insulin may cross the blood-brain barrier from the periphery into the brain region. This insulin transport may be impacted by multiple factors, such as:
- Hormones like the stress hormone, cortisol
- Certain fasting or re-feeding states
- Obesity
- Aging
- Conditions such as diabetes and Alzheimer’s disease
According to data collected in multiple studies, it's also possible that insulin may be produced locally in the brain or central nervous system.
What is the Function of Insulin in the Brain?

In the brain, insulin has a number of important actions. As mentioned above, these two main functions be broken down into two main categories:
- Supporting cognitive function, including memory and mood regulation
- Regulating food intake, hunger, and appetite
Let’s break these down into more detail below!
Cognitive Function and Mood Regulation
Insulin secretion can impact cognitive function and mood through influencing how neurotransmitters are produced and regulated in the brain. Neurotransmitters are chemicals that allow different parts of the body to communicate with one another.
Studies show that insulin can impact memory and learning in the brain and that insulin concentrations that are either too low or too high can negatively impact these processes and even lead to mild cognitive impairment.
Insulin can impact how those chemical changes occur, even leading to cognitive decline over time. In cases of insulin resistance in the brain, neurons may not respond properly to insulin’s signals.
Neuronal Survival and Plasticity

Too much insulin may be just as damaging to brain health as too little. Healthy insulin levels help protect the neurons and support healthy glycogen levels in the brain.
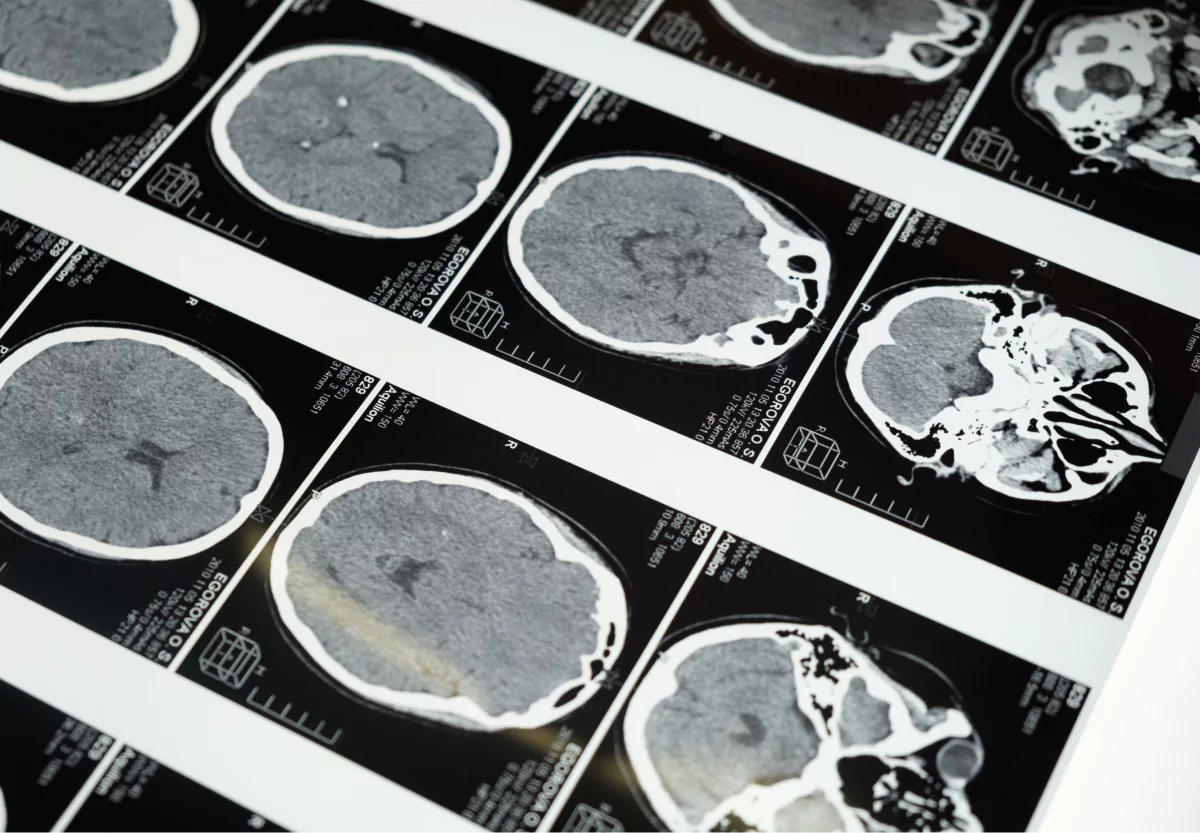
Animal studies have shown that increased glycogen may provide a buffer against brain injury during stroke or ischemia. Those experiencing acute ischemic stroke may also develop hyperglycemia.
Though more clinical trials are needed to determine the proper dosage and duration of insulin therapy in stroke patients, many researchers have recommended insulin for use in this group during the acute and early phase of a stroke to help protect from brain injury.
This is why one possible outcome of insulin resistance is an increased risk for dementia or Alzheimer’s disease and neurodegenerative disorders.
The Connection Between Insulin and Alzheimer’s Disease
But what about insulin’s role in protecting against Alzheimer’s or dementia? Insulin’s protective role doesn’t end at acute events such as stroke. Many studies have demonstrated that defective insulin signaling is a risk factor for Alzheimer’s disease and dementia.
Specifically, increased insulin resistance occurring in the brain may increase this risk. Some have proposed a new name for brain-related insulin resistance, dubbing it type 3 diabetes.
Type 3 diabetes is not currently a formal medical diagnosis and more research is needed before it might be adopted as such. Still, many researchers have suggested this term to describe a state that relates to a chronic insulin resistance alongside insulin deficiency in the brain.
The risk for dementia is increased for those with Type 2 diabetes mellitus, however. Researchers say that the increased risk of dementia in type 2 diabetes and obesity could be linked to chronic hyperglycemia, oxidative stress, increased inflammation, and microvascular disease.
Regulating Hunger and Appetite

We often think of the liver and pancreas as primary areas of the body involved in glucose homeostasis—and they are! But did you know that the brain also controls this process?
Insulin signaling in the brain may impact how other parts of the body regulate glucose. Research suggests that increased insulin resistance in the brain may contribute to hyperglycemia in some people.
There are specific clusters of neurons involved in the hunger and satiety signals coming from the brain. This means that insulin levels in the brain can have a hand in how hungry we are and when or how we eat.
The hypothalamus, for example, is the region in the brain that coordinates many functions with the endocrine or hormonal system of the body. In studies using diabetic mice, researchers saw insulin resistance occurring in the hypothalamus. This opens up new paths to explore how insulin works in the human brain, especially in those with diabetes.
Factors that Affect Insulin Levels in the Brain

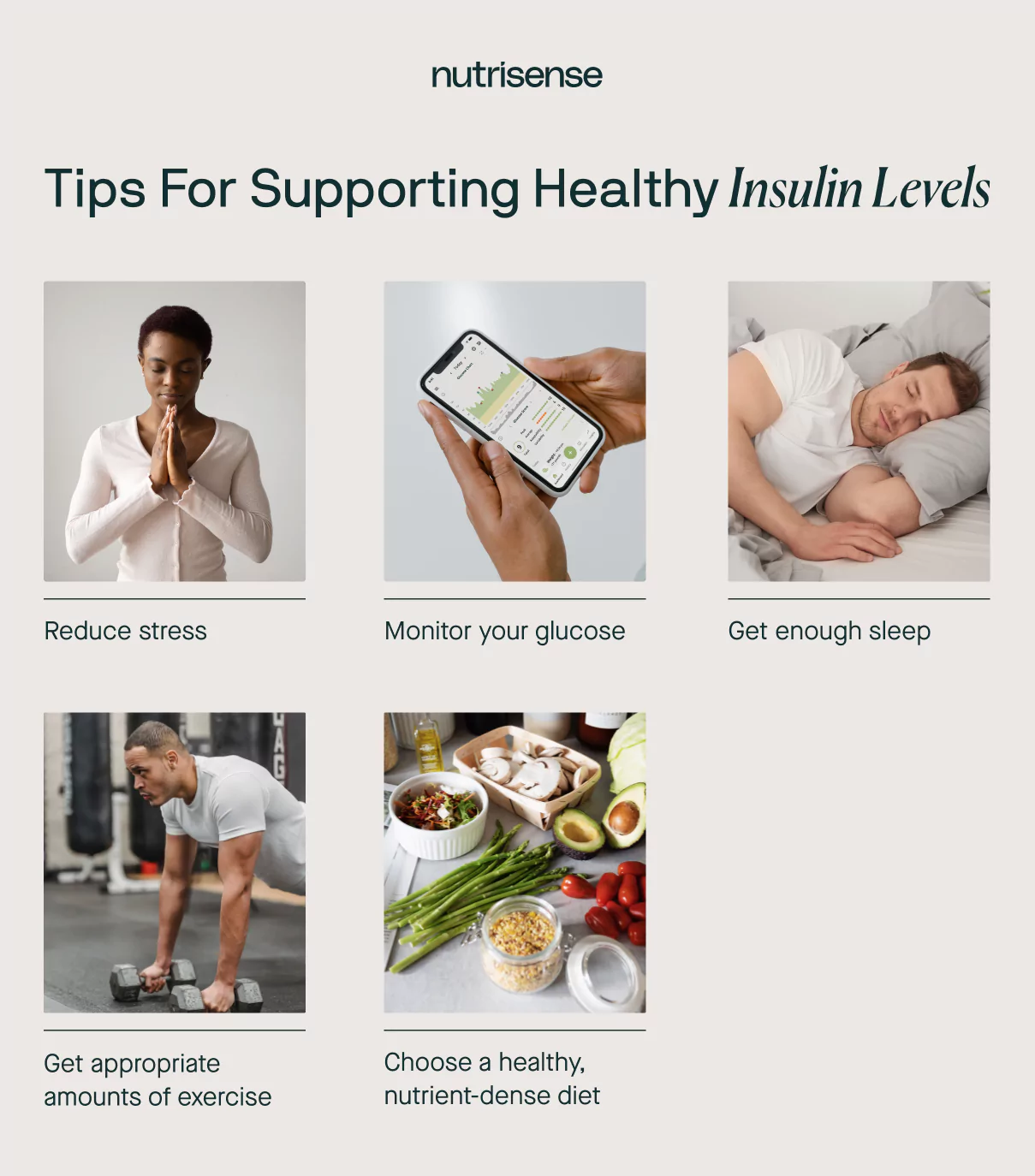
As you now know, healthy levels of insulin in the brain are important for many reasons. Insulin levels that are either too high or too low may negatively impact how the brain works. The following factors have been shown to impact insulin signaling in the brain and body:
- Nutrition
- Physical activity
- Sleep
- Stress
Genetics
So what can you do to support healthy insulin levels in the brain? Researchers are still working to uncover all the secrets of insulin action in the brain.
However, some studies have shown that healthy levels of insulin sensitivity in the body tend to correspond to healthier glucose uptake and metabolism in the brain. This means that putting effort into building healthier lifestyle habits may be one of the best ways to reduce your risk for cognitive conditions such as Alzheimer’s disease or dementia.
How To Support Healthy Insulin Levels in the Brain
Just because you might have a genetic or family history of Alzheimer’s disease or type 2 diabetes, doesn’t mean there’s nothing you can do to influence your risk of developing these conditions. Studies show that lifestyle choices and behaviors are strong predictors of whether or not you may be faced with one of these diagnoses down the road.
Below are some of the top ways you may be able to support healthy insulin sensitivity throughout your entire body (including the brain)!
Choose a Healthy, Nutrient-Dense Diet
Customization of your diet is often necessary for optimal results and working with a qualified dietitian or licensed nutritionist can give you a leg-up in finding those answers. However, there are some more general places to start that are likely to still give you a big bang for your buck.
Reduce your intake of ultra-processed foods
These may include packaged baked goods and snacks, sodas, sugary cereals, refined flour products, and other ready-packaged meals containing many food additives. These foods often contain high levels of added sugar, fat, and/or salt, but lack balanced amounts of other nutrients.
Avoid excessive alcohol intake

While small or moderate levels of alcohol intake may be associated with improved insulin sensitivity for some, higher amounts of regular alcohol intake may raise risk for insulin resistance. The effect of alcohol on your body and your risk may also be influenced by your age, family history, and genetics.
Eat a nutrient-dense diet based on whole foods
Reducing reliance on processed foods means increasing your reliance on whole foods. Making sure you meet your protein needs, get enough essential fatty acids, and hit the sweet spot of vitamin and mineral intake is a lot easier to accomplish with a whole foods-based diet.
Get Appropriate Amounts of Exercise

Making sure to get the right amount and type of exercise for your individual needs can help support insulin sensitivity. A large body of research has shown that exercise may increase insulin sensitivity.
Focusing on strength training may be particularly helpful for improving insulin sensitivity. But more exercise isn’t always better.
Overtraining or over-exercising can add more stress to your body and may even impair glucose metabolism. Overall, to get the most from your workouts, it’s important to tailor your exercise approach to your unique body.
Consider working with a professional sports dietitian, such as one of our sports-focused Nutrisense dietitians, to help you dial in your workouts. Always consult with your doctor before beginning any exercise program.
Get Enough Sleep
Researchers have found that missing out on sleep may increase your risk of developing dementia. Inadequate sleep may reduce insulin sensitivity and promote insulin resistance as well.
It’s important to remember that how and what you eat can also impact your sleep. If you struggle with poor sleep regularly, talk to your doctor and consider working with a qualified nutrition expert as well.
Reduce Your Stress

High chronic stress levels are a risk factor for developing insulin resistance. And don’t forget—stress can come in many forms. Not only is psychological or socio-emotional stress something to get a handle on, but so are other sources of stress such as:
- Poor nutritional balance
- High intake of stimulants, such as caffeine
- High intake of alcohol
- Foods, supplements, or medications your body may not be tolerating well
- Long periods of fasting that your body may not be tolerating well
- Poor sleep
- Too little or too much exercise for your individual body’s needs
If you want to gather some extra tips to manage stress, take a look at our piece on healthy ways to relieve stress.
Monitor Your Glucose

Understanding how your personal glucose levels are responding to your diet, exercise, sleep routines, and stress levels can be game-changing. With continuous glucose monitoring technology, you’re able to see your glucose in real-time and make meaningful and impactful changes to your approach.
Even a relatively small amount of time spent monitoring your glucose can offer profound insights into personal patterns and their impact on your metabolic health.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Jordyn has a bachelor’s degree in biology, a graduate degree in Human Nutrition and completed a dietetic internship at the Memphis VA. She's a dietitian at Nutrisense, and has experience working as a clinical dietitian at a VA medical center specializing in oncology and at the Mayo Clinic, working with a wide range of patients ranging from neonates in the NICU to adult ICU.


.webp)

