6 Popular IBS-Friendly Diets

Key Takeaways
It is estimated that 10 to 15 percent of adults in the United States have IBS, a chronic disease that affects the gastrointestinal tract. If you’re one of them, you know that the condition can be frustrating and painful.
While symptoms can vary from person to person, some of the most common ones include abdominal pain, diarrhea, and constipation. These symptoms can be caused by several factors, including changes in gut motility and abnormalities in the way the gut interacts with the nervous system.
Living with Irritable Bowel Syndrome

Though there is currently no cure for IBS, treatment focuses on managing these symptoms, making lifestyle changes, and reducing associated discomfort. It may involve dietary changes, medication, and stress management techniques.
Ultimately, living with IBS requires a multi-faceted approach involving medical treatment and self-care strategies to help you manage your symptoms and maintain your quality of life. Since it’s related to your digestive system, one way to deal with it is to find a diet that works best for your individual needs.
If you add or eliminate food without consulting a professional, you may experience an overly restrictive diet that could lead to undereating and not meeting your nutritional needs. So while avoiding triggers and eating foods to ease your symptoms will help, remember that if you have (or suspect you may have) IBS, it’s crucial to consult with a healthcare professional. Consider speaking with a primary care doctor, gastrointestinal physician, or a credentialed dietitian or nutritionist to find the appropriate treatment and management strategy.
General Dietary Guidelines For IBS
The best diet practices for IBS vary from person to person. However, some general dietary guidelines can help to relieve symptoms. First, eating regular meals and snacks is a better idea than skipping or waiting too long in between meals for most people. It helps prevent the overproduction of stomach acids.
Avoiding trigger foods may help to reduce intestinal discomfort. Some common ones are high fat or fried foods and foods high in insoluble fiber like wheat bran and some nuts. In addition, eating small meals and avoiding carbonated beverages throughout the day can help to prevent bloating and gas.
Some people also find relief by following a low FODMAP diet, which eliminates foods that contain high amounts of FODMAPS, which are specific types of carbohydrates and are found in a variety of foods.
While there is no one-size-fits-all solution for IBS, following some of these tips can help ease your symptoms and improve your quality of life. Ultimately, the best diet for IBS is the one tailored to suit your specific needs.
6 Popular Diets That May Ease IBS Symptoms
For people with irritable bowel syndrome, or IBS, navigating a balanced diet can be a real challenge. Some foods can trigger symptoms like bloating, cramping, and diarrhea, while others may offer more relief.
While there is no single "right" IBS diet, it’s clear that different diets may have different effects on your symptoms. The best way to find out what works best for you is by seeing how your body responds to various foods and diets. Try keeping a food journal where you can track your symptoms as a tool and work with a credentialed dietitian or nutritionist to see what will work best for you.
In the meantime, learn more about seven of the most popular IBS-friendly diets.
1) Low-FODMAP Diet
One popular approach to eating for IBS symptom relief is to follow a ow-FODMAP diet. FODMAP stands for Fermentable Oligo-saccharides Disaccharides Monosaccharides and Polyols; these are types of carbohydrates that can be difficult for some people to digest.
In short, FODMAPs are short-chain carbohydrates that the small intestine can poorly absorb. Large quantities of FODMAPs in the diet can often lead to bloating. This is caused by their ability to draw water into the intestine and by excessive gas production relating to our inability to digest them properly.
By limiting the intake of high-FODMAP foods like garlic, apples, onion, and some beans, you may notice better control over your IBS symptoms. While everyone is different, many people with IBS find that limiting the amount and frequency of high-FODMAP foods may help to reduce symptoms.
2) Gluten-Free Diet
One popular choice for those living with IBS is a gluten-free diet, which excludes foods that contain the protein gluten. Even though those with IBS don’t necessarily suffer from celiac disease, this diet may improve symptoms for some.
A gluten-free diet for IBS sufferers has several potential benefits, including reduced bloating and gas, improved digestion, and lower inflammation levels.
Identifying and eliminating certain trigger foods, such as refined bread and pasta, may help to alleviate GI distress in those with IBS. It is important to determine these triggering foods in an attempt to create a diet based on your individual needs without restricting too much.
When making dietary changes, like adopting a gluten-free diet, it can be challenging at first. However, benefits like symptom relief may make it worthwhile.
Something interesting to note here is that the reason many people see improvements in their IBS symptoms when avoiding gluten is because these foods are often high FODMAP as well.
3) Ketogenic Diet
A ketogenic diet, often abbreviated as a "keto diet," is a popular dietary approach that is often used in many different health conditions, including irritable bowel syndrome.
The basic principles behind a keto diet are simple: it focuses on consuming high amounts of healthy fats while restricting carbohydrate intake. It leads to the increased production and use of ketones, which are byproducts of fat metabolism that serve as an alternative energy source for the body.
Interestingly, several studies have found that this energy source change can help alleviate many common IBS symptoms, such as abdominal pain, bloating, and diarrhea.
Although research is ongoing, and we don’t yet know how this symptom relief works exactly, there is some evidence to suggest that a keto diet may be a useful tool in combating gut issues like IBS.
4) High Fiber Diet

A diet rich in soluble fiber (around 25 to 35 grams per day, according to this review) is often recommended as a treatment for IBS, as fiber can help to regulate bowel movements and ease symptoms of constipation and diarrhea.
However, not all types of fiber are alike. Soluble fiber dissolves in water and can be found in most fruits and vegetables, oats, and legumes. Insoluble fiber does not dissolve in water and can be found in wheat bran, whole-wheat bread, and nuts.
According to the NIH, soluble fiber is typically a good option for people with IBS as it’s less likely to cause bloating and gas. Insoluble fiber may worsen your symptoms.
When you’re increasing your fiber intake, it’s essential to do so gradually to avoid worsening symptoms. Adding too much fiber into your diet too quickly can lead to gas, bloating, and intestinal discomfort.
5) Elimination Diet
An elimination diet is a strategic way to remove potential trigger foods from your diet. It’s pretty simple in theory—you determine the foods that aggravate your symptoms and then eliminate them.
But the idea here isn’t to cut any suspected trigger foods out of your diet for good. The idea is to eliminate them for a period of time, then slowly reintroduce them one at a time in order to identify the culprits. Common trigger foods for IBS include fried fatty foods, processed and refined foods, lactose, artificial sweeteners, and high FODMAP-containing foods.
The elimination diet is often used as a way to identify food sensitivities. However, it should be noted that you should only adopt the diet under the guidance of a healthcare professional.
Eliminating foods from your diet can lead to nutritional deficiencies, so it's essential to ensure that you’re still getting all the nutrients you need.
While an elimination diet can be challenging, many find that the benefits, especially confidently identifying your dietary triggers, is worth the effort. By eliminating these potential triggers, you can ease your symptoms and get your life back on track. If you think an elimination diet might be right for you, talk to a healthcare professional like a gastroenterologist, credentialed nutritionist or registered dietitian to get started.
6) Low Fat Diet

A low-fat diet may benefit IBS patients by easing IBS symptoms. And in general, a low-fat diet may promote healthy digestion for some by reducing the strain placed on your gut by excessive fat intake.
The diet may help decrease bloating and gas and other unpleasant side effects of IBS. Overall, adopting a low-fat approach to eating can be an effective strategy to help manage IBS symptoms and improve overall well being.
{{rich-text-cta-wl2="/style-guide"}}
IBS-Friendly Kitchen Staples
If you have irritable bowel syndrome, you know that what you eat can greatly impact your symptoms. Some foods can trigger cramping, bloating, and diarrhea, while others can help to reduce inflammation and promote regularity.
Here are a few kitchen staples that people with irritable bowel syndrome should consider keeping in their pantry.
- Foods high in soluble fiber, as tolerated, such as most fruits and vegetables, and whole grains like oats. Soluble fiber helps with bowel regularity and can be appropriate for those with IBS. Foods high in fiber, such as fruits, vegetables, and whole grains.
- Low-fat proteins, such as lean meats, tofu, and fish. Fatty foods can exacerbate IBS symptoms, so it's best to limit your intake of these foods.
- Gentle fiber supplements, such as Metamucil® or Citrucel®. These can help relieve constipation, one of the most common symptoms of IBS. Remember, it’s best to consult with a healthcare professional before taking any laxatives.
- Probiotic-rich foods. Probiotics are beneficial bacteria that live in the intestinal tract. Probiotics help balance the bacteria in your gut, which can help reduce IBS symptoms. They can help improve digestive function and can be found in foods like yogurt, kefir, sauerkraut, kimchi, and other fermented foods.
By stocking your kitchen with these staples, you can make mealtime less stressful and help to control your IBS symptoms.
Foods To Avoid If You Have IBS
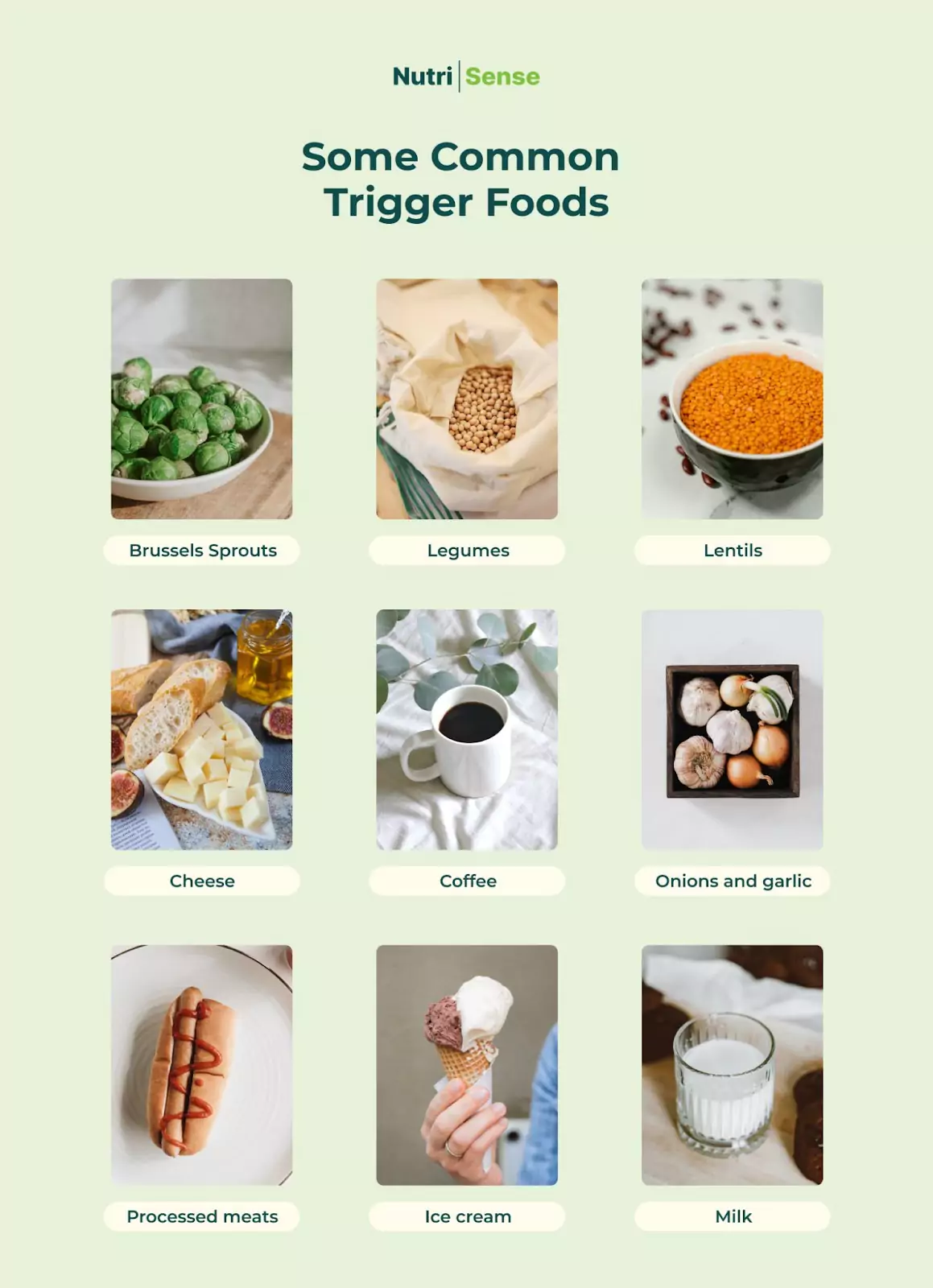
If you have irritable bowel syndrome (IBS), you likely already know that certain foods can trigger your symptoms. Everyone's triggers are different, and it’s best to speak with a credentialed dietitian or nutritionist to learn more about yours. Here’s a handy chart with some common trigger foods.
Your Menstrual Cycle and IBS
The relationship between your menstrual cycle and IBS symptoms can be complicated. The hormonal fluctuations throughout your cycle may contribute to the occurrence and severity of IBS symptoms like gas, bloating, constipation, or diarrhea.
However, the relationship between these two conditions is not always straightforward. Some women with IBS report that their symptoms are worse during their period, while others experience an improvement in their symptoms during this time.
Additionally, some women find that specific phases of their menstrual cycle don’t affect their IBS symptoms at all. Overall, it can be challenging to determine how your menstrual cycle affects your experience with IBS. The key is to pay close attention to how you're feeling and make any necessary adjustments to help manage your symptoms throughout the month.
Medicine and IBS
If you have irritable bowel syndrome (IBS), you know that managing your symptoms can be a challenge. And while symptom management usually includes dietary and lifestyle changes, you may also have to pay attention to the medication you’re taking.
While some medicines and supplements may actually make IBS worse, others may help to relieve IBS symptoms. Common medications and supplements used to help those with IBS include fiber supplements (Miralax®, SunFiber, Benefiber), laxatives (Dulcolax®, milk of magnesia), secretagogues (Imodium), antidiarrheals (Amitiza®, Trulance®), antispasmodics (Bentyl®, Levsin®), and antidepressants (TCAs, SSRIs).
For instance, fiber supplements can help reduce constipation, while antispasmodic drugs can lessen abdominal pain and cramping.
Talk to your doctor before starting or stopping any medication, especially if you have irritable bowel syndrome. With their help, you can find the best way to manage your IBS.
Stress and IBS

It’s no secret stress negatively affects your health and wellbeing. It increases feelings of anxiety and depression and can also exacerbate certain conditions like irritable bowel syndrome (IBS).
People with IBS are often highly susceptible to stress, and chronic stress can cause a flare-up of symptoms like abdominal pain, diarrhea, or constipation. Making lifestyle changes along with implementing relaxation techniques as a way to reduce stress is an important approach to alleviating IBS symptoms.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Natalie received her degree in Dietetics from Mansfield University and a Master’s in Clinical Nutrition from the University at Buffalo. Her career has included nutrition education and program development in her local community, adjunct faculty at several collegiate institutions, and clinical nutrition in both inpatient and outpatient settings.




