Prediabetes in Midlife Women Explained by Experts

Key Takeways
What Should Midlife Women Know About Prediabetes?
Continuing their insightful conversation from the first installment of this two-part interview series, Catherine Staffieri, MS, RDN, and Dr. Kathleen Jordan, MD, focus on essential but frequently overlooked health concerns during midlife, including prediabetes.
Read on for more about conditions like prediabetes during menopause, the link between lifestyle, dementia, and women's health, and more about how women can move through this important stage of life.
Catherine: There's so much to dive into when we discuss this midlife transition, and so much more is connected to it than people realize. I want to focus on those 'hidden' things: what people aren't connecting the dots to yet, beyond the lifestyle factors and hormonal changes we dove into earlier.
Kathleen: Definitely. And more specifically, I want to return to something you alluded to that I'm also seeing with many women I speak with.
Prevalence in Women
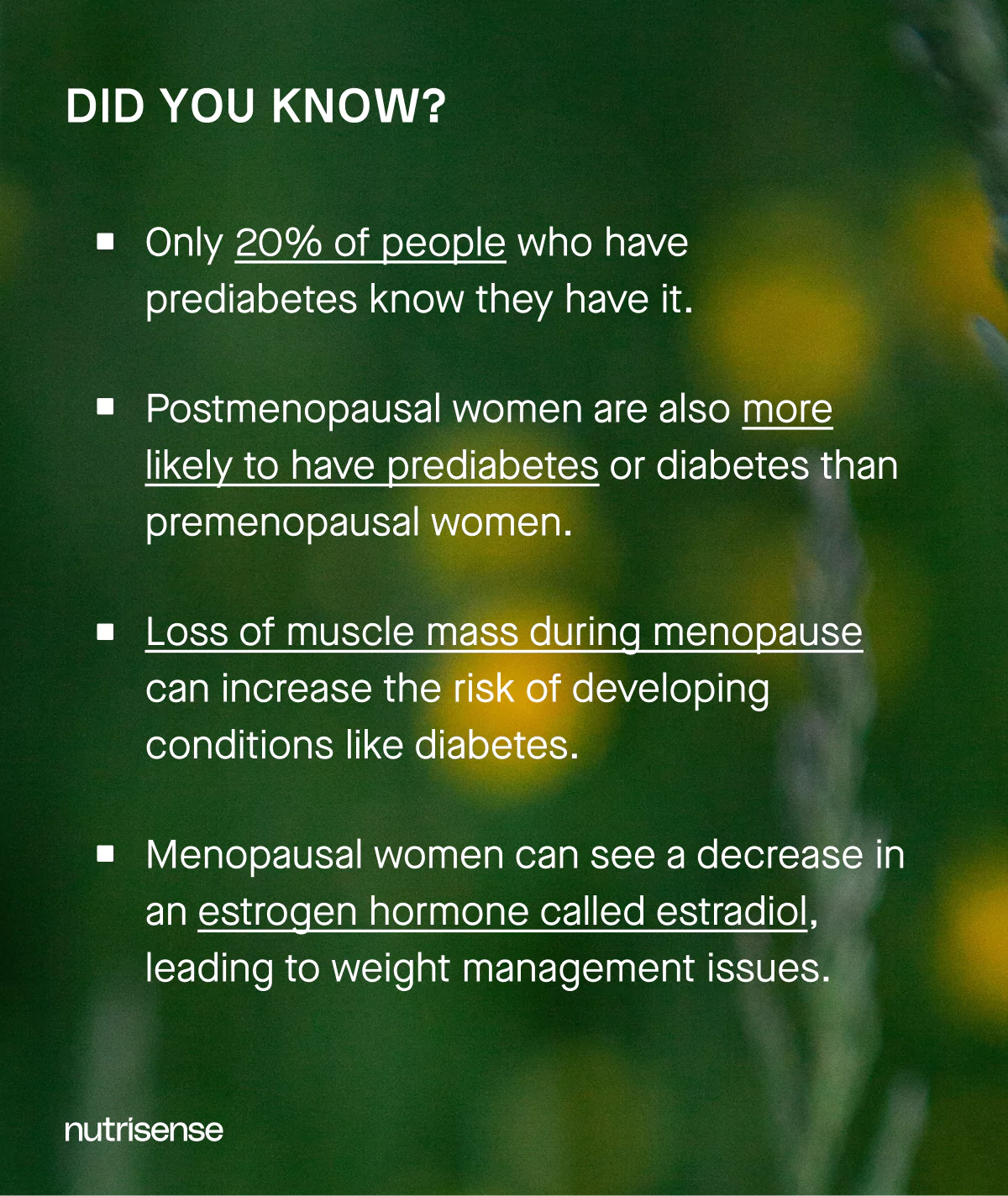
A lot of women come in with prediabetes. We know it's anywhere from a third up to 40 percent in some demographics of women who have prediabetes.
What's even more surprising is that it shows up in the bloodwork, but for many patients, their clinician hasn't told them!
Low Awareness
So, only 19 percent of people who have prediabetes know about it. So we should not only know what our data is, but we also need to understand it. To do this, we have to be adequately supported and counseled.
Prediabetes Testing and Diagnosis
Prediabetes is identified by standard lab ranges. Current guidance defines it as any of the following ranges, often confirmed with repeat testing for accuracy. See the ADA Standards of Care in Diabetes for clinical details and thresholds in adults, including midlife women.
- A1C 5.7 to 6.4 percent
- Fasting plasma glucose 100 to 125 mg per dL, termed impaired fasting glucose or IFG
- Two-hour value of 140 to 199 mg per dL during a 75-gram oral glucose tolerance test, termed impaired glucose tolerance or IGT
The oral glucose tolerance test (OGTT) challenges your post-meal response and can reveal IGT even when fasting values look normal, which is helpful when A1C or fasting results are borderline or symptoms tend to occur after eating.
Between lab checks, a continuous glucose monitor can help you see daily patterns of glucose measured in interstitial fluid, such as post-meal rises and overnight trends. Learn how a CGM works and how the Nutrisense app visualizes this data in one place.
How Can a Continuous Glucose Monitor Help in Midlife?
Prediabetes means you're in a sort of warning zone where you have a very, very high chance that you will develop full diabetes.
Diabetes is something we can live with, but it has a significant impact on health. So, when you are in this prediabetes phase, it's a super important time to lean into mitigating risks. It’s also a pretty great time to have a tool like a continuous glucose monitor!
Lifestyle Adjustments
Catherine: Oh, yes. At Nutrisense, we also look at the data and want to encourage lifestyle and behavior change in these stages. So you can make changes that last forever, but we're not against supplements either, of course.
Do you follow a similar method when talking to your patients about this? We're always trying to connect the dots: it's not just glucose, just diabetes... there's also, like you said earlier, an increase in cancer risk, an increase in heart disease. Heart disease is still the number one cause of death for women.
You have to link those things people have siloed thinking about, empower and educate them on all the health risks.
How Does Prediabetes Connect to Heart Health and More?
Kathleen: I like to use the phrase “optimizing your health.” So if you have prediabetes, you don't have full diabetes, but you're still at an incremental increased risk.
It's a period where I would like to work with you to optimize your blood sugar, but it also means I want to optimize all the systems in your body that are impacted. It's a good time to optimize all your cardiovascular risks.
Cardiovascular Screening
You need to get screened for hypertension, you need to focus on your weight, you need to optimize your diet and your cholesterol levels, and you should be focusing on some kind of regular exercise program.
Sleep and Stress
Then there's sleep and stress management with your hormones - there's no shortage of things to discuss. It's really about figuring out what you can weave into your lifestyle and what your most significant risks are.
How Do Lifestyle Habits Relate to Dementia Risk?
Catherine: And for women specifically, it's not just the prediabetes diagnosis leading to diabetes that's the only risk.
They may have genetic risks or a family history of Alzheimer's, dementia... You need to make it relevant for them to motivate them to make those changes.
I'd love to hear your thoughts on recent research about women and dementia and lifestyle factors.
Kathleen: One of the most significant risks for dementia is old age. So if we live long enough, it is something we’re likely to battle.
Women typically live longer than men, so women are twice as likely as men actually to have issues with cognitive decline. In midlife, we're also seeing our parents and their friends have issues.
We get many questions on what you can do now to prevent it. There are evidence-based lifestyle changes you can make. First, there are vascular influences on dementia. It's called vascular dementia.
Vascular Connection
Mitigating all your cardiovascular risks helps prevent dementia as well. So, all the same things we were talking about with heart attacks and stroke prevention also can help prevent dementia.
Exercise and Social Ties
There's research on vitamins and supplements, and vitamin E is the best studied in this context. There's a lot of information about how exercise can help prevent dementia. And social interaction helps, too! I think it's probably multifactorial.
With Alzheimer's, you want to know that it's happening early so you can try to slow the progression.
Screening Options
With all this in mind, for women in midlife that we see who are concerned about dementia and Alzheimer's or with high family risks, we have them do a screener called NeuroTrack. It's all just so interconnected. It's not just about “hormone changes.”
What Barriers Keep Women From Getting Midlife Care?
Catherine: Again, some people are more aware of this kind of thing and all the factors involved, only by caring for aging adults in midlife.
It's helpful to have access to support, awareness, and education to prevent all of it from developing at least 10 years earlier than we usually do.
Access Challenges
Kathleen: Nothing in healthcare is easy, I have to say. I just spent a day navigating basic screening tests myself; it's a lot between insurance, long waits, and limited access. It's difficult.
This is another reason we started Midi: to make access easier. Telehealth makes it easier, but we also make sure appointments are easy to access.
Catherine: That's so important, too. How do you do that?
Kathleen: If there's ever more than a two-week wait in a state, we have a whole operational shift in recruitment to support timely access. We are committed to timely access.
Catherine: I think that's fantastic. Because it goes back to exactly what we all want, which we also touched upon earlier:
“Women want to feel seen. They want to be seen. They want to feel heard.”
They don't want to feel like they're crazy anymore. We're all feeling the same thing at this stage: you don't feel like yourself, everything isn't working the same way it used to, it's like you've lost control of your body...
Kathleen: Right, because often you haven't changed anything, but somehow you’re getting different outcomes.
Vague Symptoms
The other barrier in midlife is that the symptoms themselves are so vague and not necessarily seen as a disease state. There's a lot of data that says 40 percent of women don't even present these symptoms to their doctor.
And then there's the second part: if they do present them, a significant number don't get the answers they need or seek.
We need women to present the problems to properly trained providers so they can actually get solutions that they can benefit from.
Conditions like prediabetes are one thing, but even before they develop, there are things connected to them that we think of as standalone issues, like thinning hair, stress, and just generally feeling exhausted.
Many women don't know how to put it into words, except that generally, every minute of every day feels hard. And that's not something women typically say to their doctor, right? You don't go to your OB-GYN and say, "I'm exhausted." But it is a symptom. So we should be saying that and expecting validated answers as well.
Catherine: Definitely. Touching on the exhaustion women feel during this stage, do you find that it's linked to thyroid, anemia, or something else that changes with changing hormones?
Common Lab Checks
Kathleen: We would send labs to look for things like that. Six percent of women have thyroid disease. Some have an iron deficiency from periods, often exacerbated by period changes. 60 percent of women say they aren't sleeping well!
Some of it is hormonal changes. So, it's generally a multimodal plan, but overall, yes, there's a lot you can do to feel better. You should not be going around feeling fatigued every day!
What Menopause Treatments Can Support Metabolic Health?
Catherine: And related to that, I'd love to hear your thoughts on Veozah, which was recently FDA-approved.
Kathleen: It's a great option. It can work for women experiencing hot flashes and night sweats. When it comes to hot flashes and night sweats, I know people joke about them, and there are always these Saturday Night Live skits on midlife women fanning themselves.
Hot Flashes Impact
They're funny, but the reality is they can impact health quite a bit. They're associated with the worst cardiovascular outcomes, including strokes and heart attacks, and they cause significant sleep disruption.
Poor sleep can have links to so many things: weight gain, daytime fatigue, conditions like prediabetes, and quality of life issues.
Hormone Therapy
Generally, we discuss different options if someone has significant hot flashes or night sweats. Hormone therapy is the most efficacious. If you look at the evidence, it is likely to work effectively and quickly.
Nonhormonal Options
But there are other options. Things like Veozah are powerful tools if, for some reason, you can't take hormones (maybe you've had breast cancer or have some clotting risks that prohibit the use of estrogens) or don't want to take hormones.
There are also other options, such as supplements and lifestyle interventions.
Catherine: It's great that people are starting to talk about it more, and the FDA approval was in the news; celebrities from Oprah to Michelle Obama are also talking about menopause...
Kathleen: People have to get comfortable with the word menopause. Half of the population goes through it, and it affects daily life. It's not a word that needs to be hidden. We can say it out loud now.
Catherine: Yes! It's fantastic that all these options are available through telehealth to help you thrive during this period.
How Does Telehealth Expand Access to Experts?
Kathleen: It's incredible. A woman could spend almost half a day going to a doctor's office, between parking, waiting in the waiting room, being seen, and commuting. You can make a telehealth appointment in 15 to 30 minutes. The accessible solution it brings for women, especially those who are really time-crunched, is impressive.
Better Visit Quality
It also gives us access to tech-enabled education tools, even as healthcare professionals. I can complete much of the intake before the visit and spend time conversing and problem-solving with the patient instead of getting their history.
So, the quality of the visit is better because I can say, "All right, I'm going to send you an article I want you to read later," and I've removed anything clerical from the visit. I can give people the best care because the tech-enabled tools can help our expert care team's suggestions.
Catherine: You're not limited by geography either, so you're not limited to just the experts in your area. That's something that's a real benefit members at Nutrisense get with our 1:1 expert support, too.
Kathleen: Absolutely. We had a woman in the Midwest who had a very complicated, rare autoimmune disorder, as well as a rare clotting issue, and she also had a lot of menopause symptoms.
Care Team Collaboration
So I had a specialist from the East Coast, a specialist from the West Coast, and a nurse practitioner in the patient's state who knew the local resources, all working together.
We had them all on the call, which took 15 minutes, and we continued that holistic approach with her care plan. That would have taken weeks, months, and thousands of dollars for her to do, and we just did it in a quick 15-minute visit. It was amazing.
Catherine: That's the home run. That's the whole point. Yeah, absolutely. That holistic approach is why we love what we do, too.
Kathleen: It's amazing to be a part of it.
Catherine: It is! Well, this has been a great chat, Kathleen. Is there anything you want to leave our readers with?
Kathleen: We're just happy to be part of solving some of the access issues for women's health and improving quality with expert-driven, evidence-based care.
And to women, I'd just say, come in sooner!
Why Act Earlier in Perimenopause?
Too many people wait well into their mid-50s to seek menopause care when they really should be seeking perimenopause care years earlier. The sooner you start, the better the outcomes. So you don't want to wait.
Catherine: Run, don't walk, to get your problem solved.
Kathleen: That's right! Thank you for what you do at Nutrisense, too. It's all interconnected!
Find the right Nutrisense programto turn insight into progress.
Prediabetes in Midlife Women FAQs
Q1. Can Nutrisense help if I am worried about prediabetes in midlife but do not have a diabetes diagnosis?
A1. Yes. The Nutrisense program pairs a CGM that measures glucose in interstitial fluid with 1:1 guidance from a registered dietitian. You will see 24/7 trends after meals, activity, sleep, and stress, then plan practical experiments that fit your routine. You can use Nutrisense with or without a diagnosis to get proactive insights.
Source: CGM without diabetes
Q2. How often do sensors in the Nutrisense program record data, and what do they measure?
A2. The sensors measure glucose in the interstitial fluid between cells and record about every 15 minutes for a continuous view of trends day and night. Use the Nutrisense app to sync readings, review post-meal responses, and compare patterns during exercise and sleep with your dietitian.
Source: How it works
Q3. What should I log in the app if I want to track perimenopause or menopause symptoms alongside glucose?
A3. Log meals with ingredients and timing, portion estimates, workouts or walks, sleep duration and timing, and notes on stress, hot flashes, or medication changes. These details help your dietitian interpret glucose responses and suggest experiments tailored to your day. You can also compare trends across different days in the app.
Source: Nutrisense App
Q4. How long should I wear a sensor to see midlife patterns in my glucose?
A4. Many members wear sensors throughout their first month to capture weekdays, weekends, workouts, travel, and sleep shifts. Sensors are typically worn for 14 to 15 days each, and Nutrisense plans include two sensors per month. That provides enough data for you and your dietitian to review trends and plan next steps.
Source: CGM Plans
Q5. Can I use Nutrisense if I am on hormone therapy or other prescriptions?
A5. Yes. The Nutrisense program can be used alongside hormone therapy or other prescriptions. It is a wellness program and does not diagnose or treat conditions. Share your medications and goals with your Nutrisense dietitian and coordinate with your healthcare provider. You can also check insurance eligibility for dietitian video calls online.
Source:Nutritionist video calls
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
Go Beyond Glucose Data with Nutrisense
Midlife brings changes like perimenopause and menopause. You may also be thinking about prediabetes and diabetes risk. Tracking a key marker, such as glucose, can make choices clearer day to day.
1:1 Expert Support
At Nutrisense, you get two things that work together: expert guidance and data you can use. Sign up to access insurance-covered video calls (coverage varies by plan) with a glucose expert. Your registered dietitian or certified nutritionist helps you turn patterns into simple next steps for meals, movement, sleep, and stress.
Track, Learn, and Act in the App
With the Nutrisense program, you can monitor your glucose using glucose biosensors and continuous glucose monitors (CGMs) that measure glucose in interstitial fluid. The Nutrisense App shows 24/7 trends and links them to your logs so you can see how dinner timing, workouts, or stress relate to next-morning readings.
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Amanda is a Nutrition Manager and Registered Dietitian, with a Masters in Dietetics from Stephen F. Austin State University. Originally from south GA, she got her undergrad degree from Texas Tech University. She worked at a hospital in Fort Worth, TX, for 4 years as a dietitian, counseling those living with HIV.



.webp)
