Causes and Symptoms of Endometriosis: What You Need to Know

Key Takeaways
Do you get severe pain during your periods? Do you also experience nausea, lower back pain, and heavy bleeding? You may think these are just the usual side effects of a ‘bad period,’ but they may signal something more. They can be symptoms of various conditions, including endometriosis.
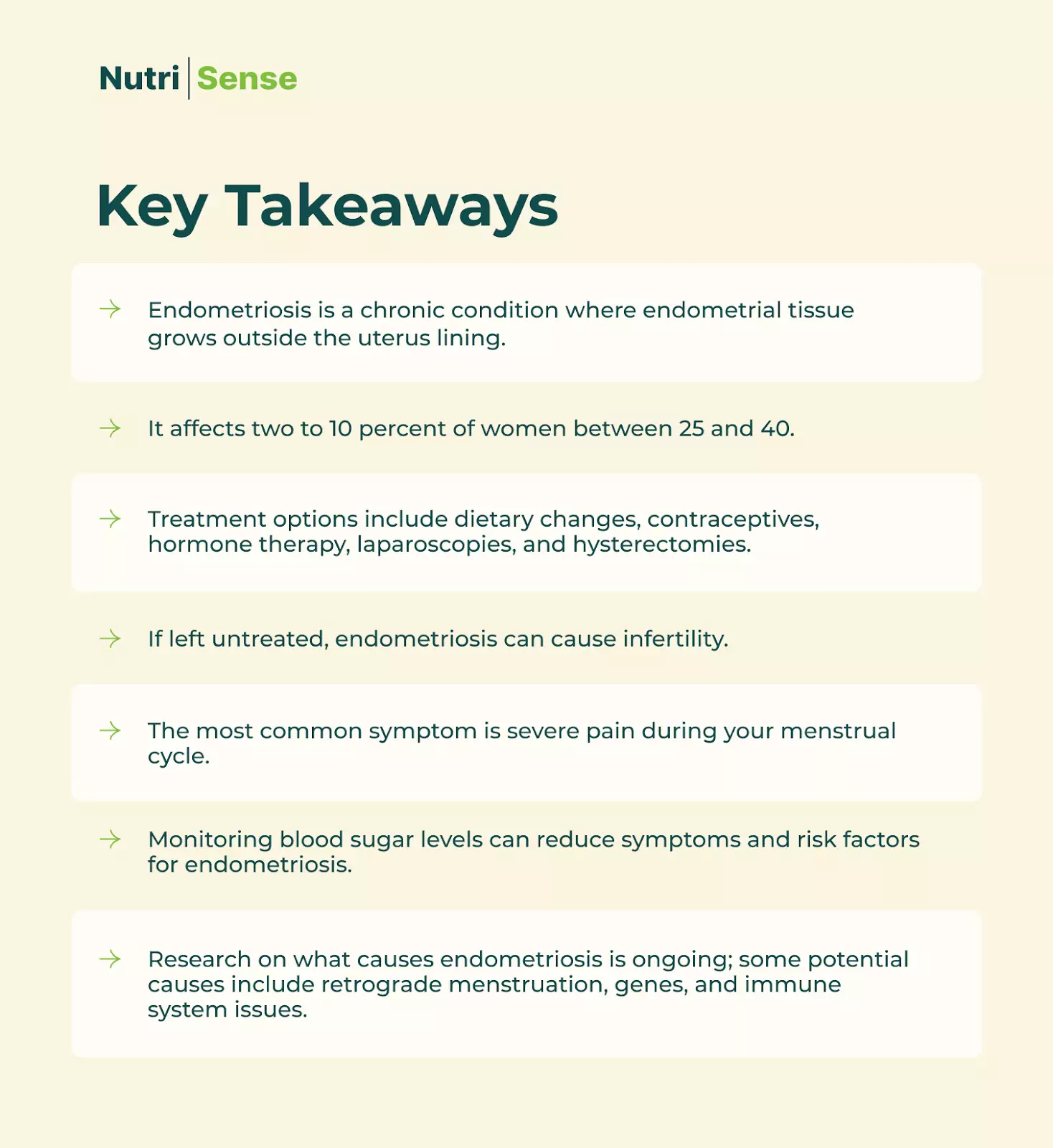
Endometriosis is a chronic pain and inflammatory condition caused by uterine tissue growing outside of the uterus that afflicts at least 11 percent of women across the world. Often dismissed as bad menstrual cramps, it has debilitating symptoms that dramatically impact your quality of life.
Since March is Endometriosis Awareness Month, we thought we’d spend some time explaining the condition and its effects on women’s health. We've also got a couple of firsthand accounts from some of our team members to shed more light on the subject. Read on to learn more.
What is Endometriosis?

Endometriosis is a chronic condition where endometrial tissue, typically on the inside lining of the uterus, grows outside it. It’s a common gynecological disease that affects women of reproductive age.
Unfortunately, like many women's health issues, endometriosis may be under-diagnosed. This can happen due to several factors, including the way many women might be unaware of the symptoms of endometriosis.
The early diagnosis of endometriosis is essential because if it’s left untreated, it can lead to infertility. If you think you have any of the symptoms, it’s important to get evaluated as early as possible.
But, since treatment of endometriosis can be as tricky as the diagnosis itself, the first and most vital step is to understand the condition.
What Are the Causes of Endometriosis?

Endometriosis occurs when the cells lining the uterus (endometrium) grow outside of the uterus. This tissue growth occurs most commonly on the ovaries, fallopian tubes, and space around the bladder and rectum. Endometriosis can cause severe pain and increase your risk factors for health problems like infertility.
Researchers and healthcare professionals are still trying to figure out the exact cause of endometriosis. They know it affects the immune cells, red blood cells, and endometrial cells, but research on the root cause of endometriosis is still ongoing.
There are three main types of endometriosis:
- Superficial peritoneal
- Ovarian
- Deep infiltrating
Peritoneal is the most common, while deep infiltrating endometriosis affects ~20% of individuals with endometriosis and is considered the most severe form. Each endometriosis subtype may have different processes of development, but no common causal thread has been determined.
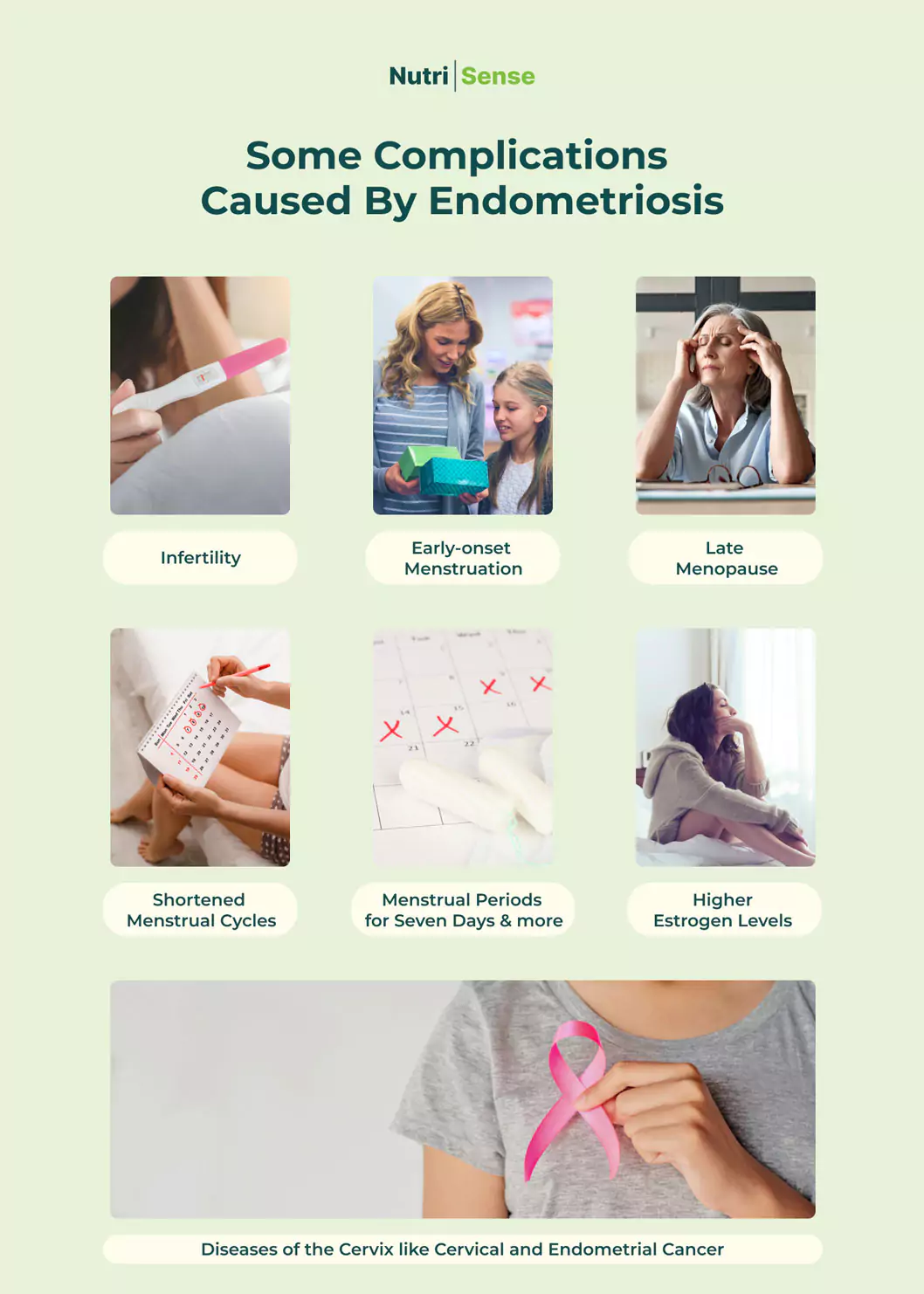
According to research, other risk factors for the condition may include:
- Having a close family member with endometriosis
- If you started having periods at an early age (before age 11)
- If you have short monthly cycles (less than 27 days)
- If you have heavy menstrual periods that last more than 7 days
Retrograde menstruation is one of the most common proposed causes. It proposes that endometriosis cells flow backward through the fallopian tubes and into the pelvis during menstruation. However, there may be many gaps in this hypothesis.
Coelomic metaplasia is another proposed mechanism, where there are changes in the cells that line the organs of the pelvis. In some studies, imbalances in gut microbiota have been connected to the altered immune function associated with endometriosis.
There are also animal studies that have shown the impact of the gut microbiota on endometriosis and endometriosis on gut microbiota more directly. Your hormones may also play a role here, as some research suggests that alteration in estrogen metabolism or other hormonal changes may be involved.
What Are Some Common Symptoms of Endometriosis?

Endometriosis affects an estimated one in 10 women of reproductive age. Although there are treatment options and ways to manage your symptoms, it’s a lifelong condition that requires daily self-care and monitoring.
Knowing some of the most common symptoms of endometriosis is an excellent first step to understanding the condition.
Common Symptoms of Endometriosis
- Painful periods. The severe pain often begins before a menstrual period and extends into the menstrual cycle. The pain may also include severe lower back and stomach pain.
- Pain during (and sometimes after) sexual intercourse. Sometimes this pain starts as a dull pain; other times, it's a severe pain that makes maintaining a healthy intimate life challenging for many women.
- Fatigue before and during the menstrual cycle. In extreme cases, this can develop into chronic fatigue.
- GI issues. Many women report stomach complications like constipation, bloating, diarrhea, and nausea during their menstrual cycles.
- Painful bowel movements and urination. This symptom is usually related to the menstrual cycle.
- Infertility. If left untreated, endometriosis can lead to infertility. Unfortunately, this is often how many women discover they have the condition.
How to Treat Endometriosis
The diagnosis of this condition can be difficult. According to current research, a laparoscopy is the only way to confirm a diagnosis of endometriosis.
Most of the standard treatments are aimed at managing symptoms. Here are some of the most common treatment options:
- Hormone therapy
- Pain medications
- Surgical treatment
Hormone therapy may involve things like hormonal contraceptives such as birth control pills. Other hormone therapy options may involve progesterone or progestin. Other drugs may be used to induce a menopausal state in the body.
Orlissa is one such drug that has been released on the market. The drug’s most common side effects include headache, nausea, difficulty sleeping, absence of periods, anxiety, depression, and joint pain.
Another drug, Danazol, has also been used. Common side effects for this drug include oily skin, acne, weight gain, muscle cramps, tiredness, smaller breasts, and sore breasts. Headaches, dizziness, weakness, hot flashes, or a deepening of the voice may also occur while on this treatment.
Danazol’s side effects are considered more severe than those from other hormone treatment options. Always consult with your doctor if you are wanting to explore treatment options.

Surgical treatments may involve laparoscopic removal of tissue associated with endometriosis and scarring. A more invasive procedure, called a laparotomy, may also be performed in some cases. A hysterectomy may be part of this procedure.
However, having a hysterectomy does not guarantee that the lesions will not return or that the pain will go away. There is still a slight chance that endometriosis symptoms and lesions may come back in some women even if they have a total hysterectomy.
There is also some promising research unfolding in using nutrition interventions to prevent and manage symptoms of endometriosis. Women with endometriosis seem to consume fewer vegetables and omega-3 polyunsaturated fatty acids and more coffee and trans fats but these findings are not always consistently replicated.
Foods that influence estrogen metabolism in different ways may be under scrutiny, though research outcomes may be conflicting. According to some studies, caffeine consumption may lead to increased concentrations of estrogen, sex hormone-binding protein (SHBG), and to lower bioavailability of testosterone.
Researchers believe this data may suggest that consumption of coffee and caffeinated beverages could be linked with the occurrence of estrogen-dependent diseases like endometriosis. Due to its ability to impact estrogen regulation and even immune function, alcohol consumption is also considered a possible risk factor.
Of all the current science looking at nutrition and endometriosis, alcohol is one of the strongest direct links to the occurrence. Other areas of nutrition will need ongoing research to confirm their role.
The Relationship Between Blood Sugar and Endometriosis

The chronic condition may also have ties to glucose regulation. Some research has shown a connection between glucose metabolism, insulin sensitivity, and endometriosis.
This may be a complex interaction and more research is needed to determine to what degree blood sugar levels are impacted by, or in turn, can themselves impact endometriosis development and symptoms.
Stories of Endometriosis Management
Dealing with and managing the symptoms of endometriosis can be an overwhelming prospect. Since the condition is under diagnosed and under researched, everything from diagnosis to treatment can be challenging. It’s a good idea to join a support group so you can talk to other women before, during, or after a diagnosis.
And, if you’re still wondering whether what you’re feeling is a symptom of endometriosis, hearing firsthand accounts can help. Here are some accounts from two members of the Nutrisense team that may be able to help.
"I was diagnosed with endometriosis in 2017, but only after emergency surgery. I spent more than 20 years menstruating, ignoring that I had the condition. I normalized that my period would leave me in unbearable pain every month. I assumed the heavy bleeding and pelvic pain were normal, and I just needed to “man up” and get on with my life.
That’s what medical professionals would say too! “Oh, you need to take birth control to ease the pain. When you become a mother, it will get better. Don’t worry, it happens….” But then a 9-centimeter cyst got infected in my right ovary, and I had a high fever for over a week.
I wasn’t even aware that a tennis ball lived in my uterus since women in my condition can develop a cyst over a short period. It got so bad that my appendix became infected too. The doctor decided to take me to the operating room after an unsuccessful four-day in-hospital intravenous antibiotics treatment.
Fortunately, my right ovary is still alive, and I said goodbye to a useless organ. But it was only after the intervention that my doctor explained that I had this incurable yet treatable condition. Raising awareness is one of the things we need to work on. So, since this is Endometriosis Awareness Month, I wanted to share my story to tell all you Endo Warriors out there—we're not alone. And, most of all, if you haven’t been diagnosed yet, to remind you—pain is not normal. Please listen to your body and find a doctor who listens to you!"
Check out more from Luz’s story on Instagram.

"I was diagnosed with endometriosis in my teens, and my diagnosis continued throughout the early part of my twenties. I underwent multiple levels of drug therapy, including chemically-induced menopause, to "treat" the condition. Unfortunately, all of these approaches led to worsened symptoms and additional medical conditions that continued advancing throughout my twenties.
After spending over a decade seeking answers from every corner of the medical world (both traditional and functional/alternative) without much progress, I was beyond frustrated and felt defeated. But I didn't give up searching for answers! It was a unique approach to customized nutrition therapy that eventually led to my successful recovery. And not only from endometriosis but other diagnoses too, including PCOS, chronic fatigue syndrome, and more.
This profound personal experience of transforming my health and regaining my hormone balance inspired me to complete my master's in nutrition science and become a dietitian to practice clinical nutrition for a living.
To date, I've worked with hundreds of women struggling with various hormonal imbalances, including endometriosis. And I've seen the incomparable power of customized nutrition offer them hope when other avenues have failed them.
Each person is unique, so what dietary approach works for one person may not work the same for another—but understanding how to navigate and customize those experiments and tools is what's important."
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Heather is a Registered and Licensed Dietitian Nutritionist (RDN, LDN), subject matter expert, and technical writer, with a master's degree in nutrition science from Bastyr University. She has a specialty in neuroendocrinology and has been working in the field of nutrition—including nutrition research, education, medical writing, and clinical integrative and functional nutrition—for over 15 years.




